By: M. Tuan Tran, infectious disease pharmacist at CHOC, and Dr. Negar Ashouri, infectious disease specialist at CHOC
With the Centers for Medicare and Medicaid Services (CMS) and the Joint Commission set to require the adoption of core elements of antimicrobial stewardship in 2017, CHOC will continue to uphold the appropriate use of antimicrobial agents through its existing antimicrobial stewardship program.
CHOC’s multidisciplinary collaborative’s goals include:
- Optimizing selection, dosing and duration of therapy
- Reducing adverse events including secondary infection (e.g. clostridium difficile infection)
- Improving patient outcomes
- Slowing the emergence of antimicrobial resistance
- Preserving supply especially during critical shortages and reduce health care expenditures
The collaborative’s strategies include:
- Pre-authorization of broad spectrum agents such as meropenem, cefepime, vancomycin, daptomycin and linezolid
- Daily review (prospective audit with feedback) of antimicrobial orders
- Development of care guidelines, dosing protocols and order sentences in the electronic health record
- Dose optimization based on PK/PD principles (e.g. prolonged infusion of beta-lactams)
- Document indication and duration for all antimicrobial orders
- Antibiotic time-out at 48-72 hours to: reevaluate need to continue treatment; streamline, de-escalate based upon culture result; convert intravenous to oral route when appropriate; reassess optimal treatment duration
- Track trends and share antibiotic utilization data as well as resistance trends
- Provide education for staff, patients and family of optimal antimicrobial therapy use
Changes to clinical practice patterns to promote the appropriate use of antibiotics is a patient safety issue and public health imperative: Antibiotics are the second most commonly used class of drugs in the United States, and studies indicate that 30 to 50 percent of antibiotics prescribed in hospitals are unnecessary or inappropriate. Further, antibiotic exposure is the single most important risk factor for the development of clostridium difficile infection.
“Through education and teamwork we can reduce the unnecessary use of antibiotics, therefore minimizing the risk of potential side effects to ensure we have effective antibiotics available for the generations to come.”
– Dr. Negar Ashouri, infectious disease specialist at CHOC
The Centers for Disease Control and Prevention (CDC) estimates that 2 million illnesses and 23,000 deaths are caused annually by drug-resistant bacteria in the U.S. alone. Avoidable costs from antibiotic misuse range from $27 billion to $42 billion per year in the U.S. At the same time, the discovery and development of new antibiotics have dropped precipitously from the 1980s onward. All antibiotics approved for use in patients today are derived from a limited number of classes of agents that were discovered by the mid-1980s (see figure 1).
Figure 1.
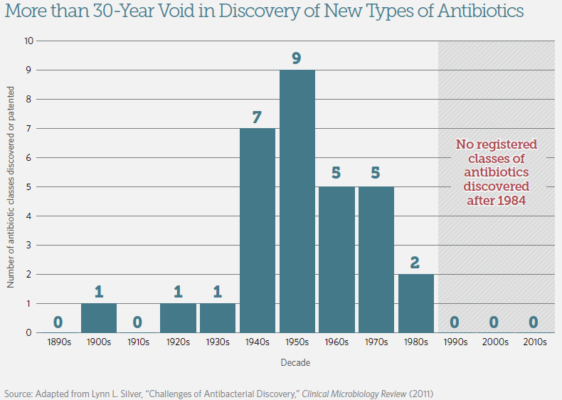
Source: A Scientific Roadmap for Antibiotic Discovery. The Pew Charitable Trusts, May 2016.
Here are some common reasons for misuse of antibiotics in health care settings:
- Use of antibiotics when not needed
- Continued treatment when no longer necessary
- Use of broad-spectrum agents when more targeted/narrower options are available
- Wrong antibiotic given to treat an organism/infection
- Incorrect dosing and frequency
Antibiotics can also affect beneficial bacteria that are part of our normal flora:
- An average child receives 10 to 20 courses of antibiotics before age 18
- Antibiotics affect microbiota flora which may not fully recover after a course of antibiotics
- Overuse of antibiotics may be contributing to obesity, diabetes, inflammatory bowel disease and asthma
For information about the appropriate use of antibiotics for your patients and families, please visit our CHOC Blog.




