To the untrained eye, the seizures are so small – “tiny little blips,” the mother calls them – that they’re difficult to detect.
The effects of the seizures, however, are devastating.
Lily Rana recently turned 4, but she doesn’t walk and isn’t verbal yet.
In addition to other health issues, she has refractory generalized epilepsy.
Medication is helping to control her spasms and she’s progressing some, says her mother, Janani, but a condition CHOC specialists diagnosed in Lily when she was 8 months old – infantile spasms (IS) – caused significant cognitive damage.
Today, CHOC finds itself at the hub of a new study involving 21 of the nation’s highest-level pediatric epilepsy centers. The research project aims to detect predictive biomarkers for infantile spasms so the condition can be treated as early as possible, which is critical to achieving optimal outcomes.

Parents like Janani are encouraged.
“Hopefully this research will help identify biomarkers that can prevent some other families from going through what we’ve been through – which, honestly, has been hell,” she says.
“When Lily first began showing signs of developmental delay,” Janani adds, “I had never heard of infantile spasms. I thought seizures were what you saw on TV – the grand mal seizures. And when I did stumble across infantile spasms in an online search, I naively thought they were something mild that could be overcome quickly. I mean, the movement is so small. I had no concept of how catastrophic they could be.”
Pediatric Epilepsy Research Foundation (PERF) awards grant to create largest database of its kind
CHOC’s Dr. Daniel Shrey, a neurologist and epilepsy specialist, knows all too well about the profound harm infantile spasms can cause.
He’s leading the research effort he says will create the largest infantile spasm database of its kind.
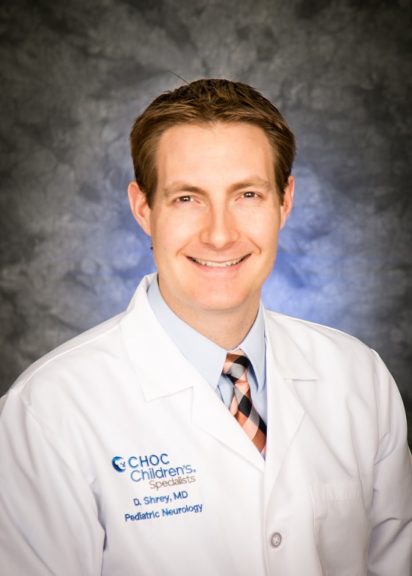
In 2021, the Pediatric Epilepsy Research Foundation (PERF) awarded CHOC a two-year, $200,000 infrastructure grant to run the multi-site study to look for quantitative biomarkers to predict the likelihood of IS.
In early 2022, a CHOC CSO grant provided the means to add four more pediatric hospitals to the project.
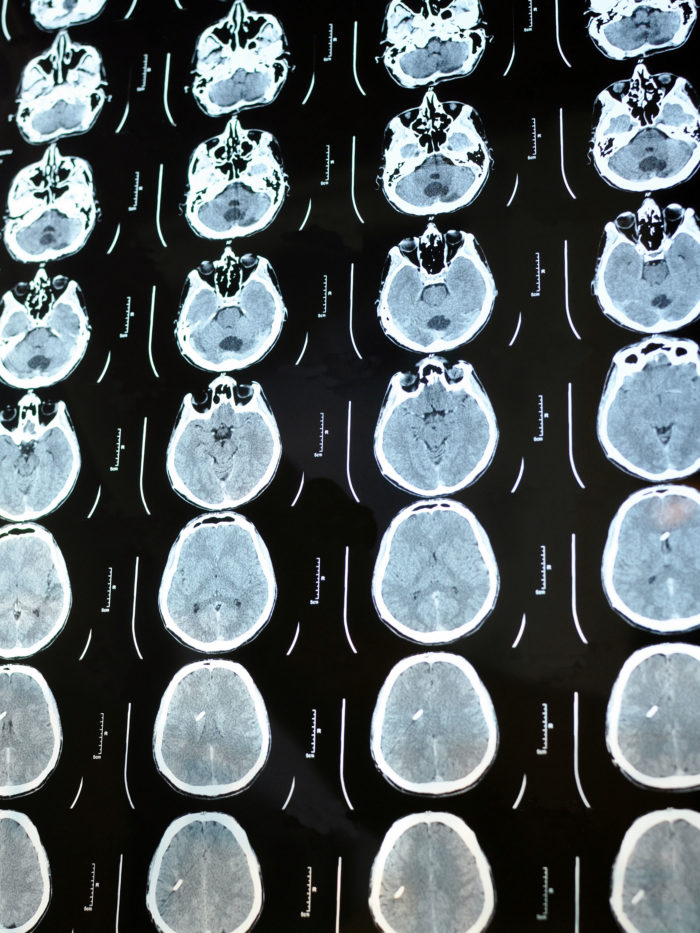
These 21 centers will collect information from 600 unique IS patient records that will be stored in a cloud-based platform so specialists can analyze EEG (electroencephalogram, a test that measures the electrical activity of the brain and is crucial for diagnosing and managing most types of epilepsy) and MRI (magnetic resonance imaging) data, among other information.
“Significant barriers to treatment of IS persist, so there’s a critical need for objective biomarkers that can identify infants with IS who are at high risk for first-line treatment failure and relapse,” says Dr. Shrey, co-principal investigator of the study along with Dr. Shaun Hussain, director of the Infantile Spasms Program at Mattel Children’s Hospital at the UCLA David Geffen School of Medicine.
The objective of the PERF study, Dr. Shrey explains, is to develop a predictive multimodal biomarker for IS based on clinical, genetic, imaging and EEG features.
The research represents the first step toward personalized treatment for IS, with patients stratified based on their likelihood of response and relapse, says Dr. Shrey. Ultimately, he adds, such research could transform the clinical landscape by improving long-term patient outcomes and lowering healthcare costs.
“These kids have a lot to lose,” says Dr. Shrey. “There’s a huge need to find ways to improve their outcomes.”
Few advances in treatment strategies for infantile spasms (IS) over the years
Over the past few decades, epileptologists have struggled to make significant strides in prediction or diagnostic abilities or even treatment strategies for patients with IS, says Dr. Shrey.
The standard treatment has been to try different medications alone or in combination.
Finding predictive biomarkers, he says, could be a game-changer for kids with IS, the most common epilepsy syndrome in the first year of life with an incidence of 2-5 per 10,000 births.
Without successful treatment, IS imparts lifelong consequences. Up to 13 percent of IS patients will die before their first birthday.
Thirty-five percent of children with IS develop autism and between 75 and 90 percent are intellectually disabled.
Less than 20 percent of children with infantile spasms will go on to live normal lives.
EEG leads to an IS diagnosis for Lily, finally
When Lily was 3 months old, Janani and her husband, Gaurang, began noticing signs she wasn’t progressing.
A series of tests and appointments with doctors, including a pediatric neurologist, turned up no clear diagnosis.
“We asked so many people,” Janani says. “Everyone kept insisting she was fine or would grow out of the delays. But something just didn’t feel right.”
It wasn’t until the couple brought Lily to CHOC that they finally got a diagnosis. It was Dr. Hussain’s infantile spasms website, which has videos of other children having movements just like Lily’s, that gave them the courage to finally seek out help from CHOC.

A 24-hour video EEG at CHOC confirmed their worst fears: Lily’s delays, which appeared to be getting worse daily, were due to hundreds of daily tiny seizures that were disrupting her brain from functioning properly.
Since her diagnosis, Lily has tried (and failed) multiple epilepsy medications, including the ketogenic diet.
Janani and Gaurang are convinced that had they come to CHOC sooner, Lily’s life would be completely different.
“Will my daughter ever call me Mom?” Janani asks herself. “Will I ever see her jump in puddles? How could we have missed this? How could so many people have missed this?”
Parent advisors for PERF IS study
Janani and her husband will serve as parent advisors on the PERF IS study.
“I think there’s an opportunity for us to connect with other parents, advise them about what we’ve been through, maybe talk about the medications we’ve experienced,” she says. “Medications can be tough not just on the children but on the parents as well. Side effects can be harsh. You need to make sure you have a knowledgeable epileptologist to guide you through the maze of seizure meds. It’s one of the reasons we’re so grateful to live by CHOC and to have Dr. Shrey as our doctor.”
In addition to IS, Lily has a possible metabolic condition, bilateral hearing loss, nephrotic kidney syndrome, and focal glomerulosclerosis.
She regularly sees Dr. Richard Chang, a metabolics specialist, and Dr. Shoba Narayan, a nephrologist. As she has no diagnosis, she also sees Dr. Neda Zadeh, a geneticist.


Dr. Shrey says he and his collaborators on the PERF IS project hope to have data collected by the end of 2022. At CHOC, data will be collected from 35 patients; each participating hospital will recruit between 25 and 45 patients.
Possible NIH study for IS biomarkers
Dr. Hussain was Dr. Shrey’s mentor when Dr. Shrey was a resident at UCLA. Since joining CHOC in 2013, Dr. Shrey has done most of his epilepsy research in collaboration with his wife, Professor Beth Lopour, and her lab at UC Irvine.
Dr. Lopour, an associate professor of biomedical engineering in the UCI Samueli School of Engineering, directs the Laboratory of Computational and Translational Neuroscience. Her research primarily focuses on EEG-based computational epilepsy biomarkers that measure characteristics of brain activity that humans can’t visually appreciate.
“What we’re hoping to do with the findings of this PERF study is to propose an NIH- (National Institutes of Health) funded biomarker study that will allow us to include other types of data like genomics, plasma inflammatory biomarkers, and other biochemical data that are not yet universally collected from infants with IS,” says Dr. Shrey, whose research relies heavily on his undergraduate degree in biomedical engineering.
“That’s where we hope it goes in the next few years.”
Staying active in the IS community
Meanwhile, Janani plans to remain active in advocating for more funding for IS research.
She served for two years on the board of the Epilepsy Foundation of Orange County and was recently a panelist at the foundation’s Enterprising Women’s Luncheon attended by several doctors from CHOC and UCI.

Dr. Virginia Liu, a CHOC epileptologist, also was a panelist at that luncheon. For Janani, the event felt very full circle – Dr. Liu was completing her residency in CHOC’s Neurology Department when Lily was first admitted to CHOC and happened to be rounding the day of Lily’s initial IS diagnosis.
Janani recalls Dr. Liu’s knowledge and compassion from that day vividly.
“Until you delve into the IS community,” Janani adds, “you don’t realize how serious this rare condition is. Most people don’t even realize it exists. Epilepsy is not an appetizing disease – it’s not pretty, and it’s not amenable to photos and videos of happy children and happy outcomes that encourage funding. And IS, a small and rare subset of epilepsy, is even less so given how many children suffer seriously adverse outcomes.
“And so, I’m yelling about IS to everybody. Maybe the right donor or right pharma company will fund IS research. The more relatable infantile spasms become, the more people will want to think about funding it. Without funding, we can neither prevent nor cure.”

CHOC Hospital was named one of the nation’s best children’s hospitals by U.S. News & World Report in its 2025-26 Best Children’s Hospitals rankings and ranked in the neurology/neurosurgery specialty.