The Comprehensive Epilepsy Program at CHOC is at the forefront of bringing precise, combined PET/MRI imaging to neurologists and their patients.
“Sometimes if we look at the PET scan and the MRI separately, we might miss a very small lesion,” says Dr. Maija-Riikka Steenari, pediatric neurologist and epilepsy specialist at CHOC. “That is why we now do precision neuroimaging for every patient we deem to be a possible epilepsy surgery candidate.”
For the subset of pediatric patients with epilepsy who need surgery to treat their symptoms, traditional neuroimaging does not always show the full extent of the lesions to be removed.
“In addition to pediatric epilepsy specialists and neurosurgeons, our pediatric neuroradiologists and advanced neuroimaging scientist, Sumiko Abe, PhD, play integral roles in the surgical decision-making process,” Dr. Steenari says. “Dr. Abe has been an essential member of the CHOC epilepsy team. Her ability to generate high-resolution 3D fusion images and segmented reconstructions has improved the outcomes and lives of some of our most complicated epilepsy patients.”
Synergy: PET plus MRI
Co-registration/fusion of PET scans with MR brain imaging increases the sensitivity for finding the seizure focus. At times, combining PET/MR fusion imaging with scalp EEG recordings is sufficient to devise the surgical plan, given the available data are concordant. However, this is often not the case. When the seizure focus is not clearly identified with non-invasive testing, or if there are eloquent brain regions abutting the presumed seizure onset zone, invasive monitoring may be indicated.
In these instances, the patient will have intracranial EEG (iEEG) electrodes placed directly onto or into the brain, to map the seizure onset zone as well as eloquent cortex. Subdural electrode grids are placed onto the surface of the brain, whereas stereotactic EEG electrodes are implanted to measure deeper brain activity. Epilepsy specialists use the iEEG data, combined with the neuroimaging data, to create a 3D map of the brain, allowing them to better understand the seizure onset zone in relation to important anatomical structures. Higher-resolution brain mapping can be accomplished by electrical stimulation, for identification and delineation of eloquent cortex.
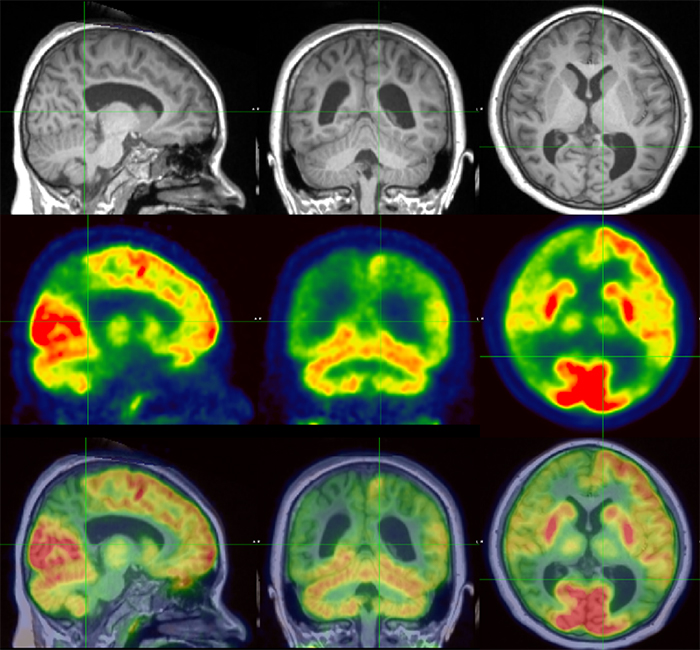
Precision brain mapping can also solve problems that were previously unsolvable.
“I had a patient who underwent a functional hemispherectomy to treat his refractory seizures,” Dr. Steenari said. “However, a year later, his seizures came back. We were able to use brain imaging tractography to delineate his white matter tracks, and we discovered a residual connection between the left and right hemispheres that had not been disconnected during his initial surgery. With this finding, our epilepsy neurosurgeon was able to go back and complete the disconnection, improving his surgical outcome.”
A guide to safer brain surgery
One of the greatest advantages of 3D brain mapping is lowering the risk of major complications after brain surgery.
“When we see where the electrodes are and we can mark where the seizures are coming from three-dimensionally, instead of looking at 2D imaging, that helps us to avoid critical areas while making sure that we remove the entire epileptogenic zone,” Dr. Steenari says.
In 2019, Dr. Steenari treated an otherwise healthy adolescent patient who was experiencing 10 to 20 seizures a day. The first physician the patient saw ordered an MRI that was initially thought to be normal. With CHOC’s advanced neuroimaging Dr. Steenari was able to identify a focal lesion known as a cortical dysplasia, making the patient a candidate for epilepsy surgery.
“Her seizures started very close to the language area in her brain, and we didn’t want her epilepsy surgery to result in a language deficit,” Dr. Steenari says. “We functionally mapped her brain’s language region by stimulating all of her electrodes one-by-one, and I was able to map out a safe resection zone where her language wouldn’t be affected.”
While the patient did have some transient motor function and language issues immediately after the surgery, occupational therapy put her back on track, including getting a driver’s permit. The patient is now seizure-free with neither language nor motor deficits.
Uses beyond epilepsy
Physicians at CHOC are also using precision neuroimaging and 3D brain mapping to prepare for surgeries to remove brain tumors and to help treat traumatic brain injuries. Beyond the minor risks of radiation exposure in a PET scan and the sedation given during an MRI, the advanced imaging is safe for children.
“At CHOC, we’re all pediatric neurologists and pediatric specialists,” Dr. Steenari says. “We always offer multidisciplinary evaluations to provide the best care for the child. We review every case as a comprehensive team, so families get the entirety of our collective expertise.”
Learn more about the Comprehensive Epilepsy Program at CHOC.

CHOC Hospital was named one of the nation’s best children’s hospitals by U.S. News & World Report in its 2025-26 Best Children’s Hospitals rankings and ranked in the neurology/neurosurgery specialty.