In a recently published research paper, a CHOC pediatric otolaryngologist predicts a “paradigm shift” in the next five to seven years to make intracapsular tonsillectomies (ITs) the standard surgical technique for removing tonsils in children either for snoring and sleep disordered breathing or for chronic/recurrent tonsillitis.
CHOC was among the first pediatric hospitals in the country to adopt ITs as its standard technique, but Dr. Kevin Huoh notes in his paper, “Current Status and Future Trends: Pediatric Intracapsular Tonsillectomy in the United States,” published in Laryngoscope, the foremost publication for otolaryngologists, and co-written by Dr. Yarah Haidar and Dr. Brandyn Dunn, both of the UCI School of Medicine, only 20 percent of the 540 pediatric otolaryngologists who responded to a survey the three doctors sent perform ITs.
“The reasons (most other ENTs) are not doing ITs are probably psychosocial,” Dr. Huoh says. “They’re not exposed to it. They’ve been doing tonsillectomies the same way for forever and they have a lack of exposure to this new procedure. Simply, they are set in their old ways.
“But this procedure is very, very favorable. It’s very easily learned, and it really works.”
Intracapsular tonsillectomies have steadily gained popularity in the United States and across the world since the procedure first was described in 2002.
Dr. Huoh brought the technique to CHOC when he started there in September 2013 after learning it during his fellowship at Stanford University Medical Center. So, too, did fellow pediatric otolaryngologist Dr. Nguyen Pham, who joined CHOC around the time Huoh did.
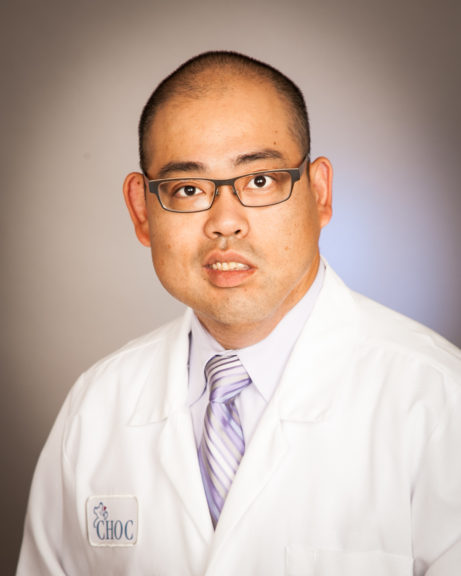
Dr. Kevin Huoh, pediatric
otolaryngologist at CHOC
Dr. Nguyen Pham, pediatric otolaryngologist at CHOC
Since then, more than 1,000 children have undergone intracapsular tonsillectomies at CHOC, with the rate of tonsillar regrowth – the most cited concern for not performing ITs – remaining extremely low, Dr. Huoh says. In addition, the rate of post-tonsillectomy bleeding, the most feared post-operative complication, is pretty much zero, much lower than with traditional extracapsular tonsillectomy.
That is certain to change in the coming years as the benefits of the technique become more widely recognized, Dr. Huoh says.
Dr. Huoh and other CHOC doctors mainly perform intracapsular tonsillectomies on children whose large tonsils cause obstructive sleep apnea.
Such was the case with Madison Boehm.
When she was 2, her parents noticed she snored a lot and woke up tired. She was sluggish and lethargic and took one or two three-hour naps per day.
“We went online and did some research, and sleep apnea popped up,” Lisa recalls.
Lisa says she and her husband, Cameron, researched the best hospital to take Madison to and they quickly settled on CHOC, where Dr. Pham diagnosed Madison as having large tonsils and adenoids as well as obstructive sleep apnea.

Madison was diagnosed with having large tonsils and adenoids as well as obstructive sleep apnea 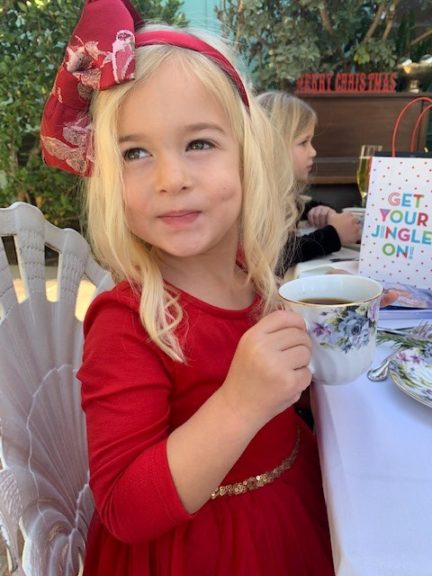
At age 3, Madison underwent an intracapsular tonsillectomy
Madison had the surgery on Aug. 3, 2019. Then 3, she had an intracapsular tonsillectomy, in which 95 percent of the tonsils are removed, preserving the “capsule,” and thus protecting the muscle underneath.
The result is less risk of postoperative bleeding, vastly decreased postoperative pain and a rapid return to normal diet.
The vast majority of the nearly 300,000 children who have tonsillectomies in the United States every year have both of his tonsils completely removed via a technique known as an extracapsular tonsillectomy (ET).
“The doctors at CHOC were all dialed in, and I was holding her an hour after she went under,” says Lisa, Madison’s mother. “The recovery part is what was amazing. By the time we were home, she was totally out of the anesthesia fog and asking to eat.”
So, Lisa got Madison a cheeseburger.
She never complained about her throat – just soreness on the top of her hand from the IV.
“She completely recovered in a couple of days,” Lisa says of Madison, who enjoys dancing and gymnastics. “From that first night after surgery, she has been sleeping normally, and I feel that her personality has come out a little more.”
Lisa says she has referred her friends who have kids with tonsillar problems to CHOC pediatric otolaryngologists.
“The doctors treat their patients like they are their own kids,” she says. “I had total confidence in them. They carefully explained everything that was needed, and I could always be in touch with them. They are second to none.”




