The Neurometabolic Program at CHOC has become the largest center in the United States and the second largest in the world to offer the breakthrough enzyme replacement therapy Brineura, improving the quality of life for children diagnosed with late infantile neuronal ceroid lipofuscinosis type 2 (CLN2), one of many neuronal ceroid lipofuscinosis conditions collectively referred to as Batten disease.
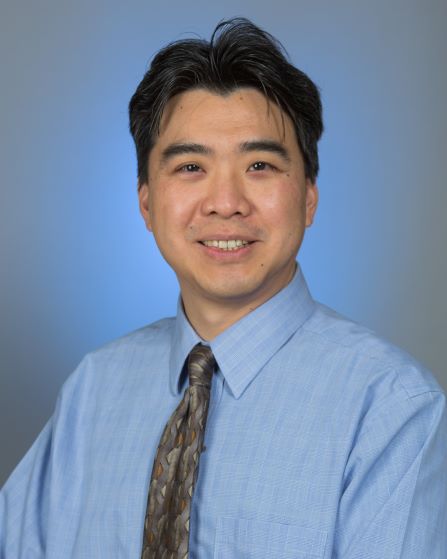
“In the past, we’ve watched children go from relatively healthy toddlers to developing epilepsy and losing most, if not all, of their developmental milestones, eventually leading to early childhood mortality,” says Dr. Raymond Wang, biochemical geneticist and director of the multidisciplinary Foundation of Caring Lysosomal Storage Disorder Program at CHOC. “With Brineura, these kids are not declining. They’re still able to walk around and interact with their parents. It’s not a cure, but it’s giving kids and their families much more meaningful time and memories together.”
A significant step forward
Brineura (cerliponase alfa) is a synthetic TPP1 protein that received FDA approval in April 2017 and represents the first major advancement in the battle against CLN2 Batten disease. Administered through intraventricular infusion, the protein is delivered to the cerebrospinal fluid, where it targets brain cells and removes waste materials. The treatment decelerates the progression of the disease, slowing the onset of symptoms, particularly the loss of ambulation. To be eligible for the treatment, children must be at least three years old and able to walk, with or without assistance.
CHOC has been providing Brineura treatments for four years. While long-term outcomes are still unknown, the benefits have been life-changing for patients and their families. While children with CLN2 disease on Brineura can still have significant symptoms, such as developmental delays, learning disabilities and epilepsy, the treatment prevents or drastically slows regression. It can also greatly reduce indicators of refractory epilepsy.
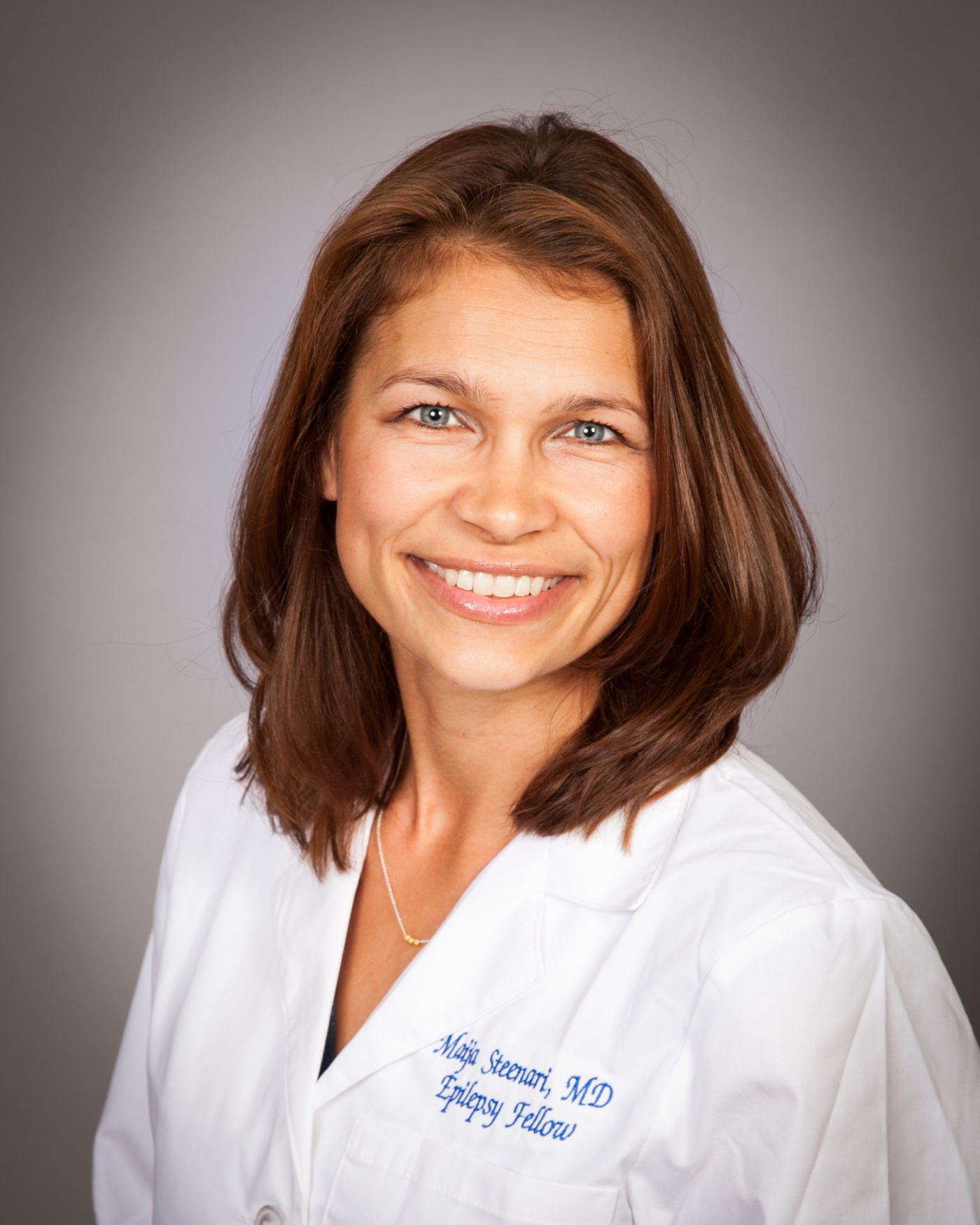
“It really improves quality of life,” says Dr. Maija-Riikka Steenari, pediatric neurologist and epilepsy specialist at CHOC. “For children who are on the treatment, their seizures are better controlled as well. Instead of having 20 seizures a day, they might have one every two months, and I can lower the doses on other anti-epileptic medications.”
Innovation and collaboration
Dr. Wang spearheaded the effort to introduce Brineura to CHOC in 2014 after diagnosing a four-year-old boy and his younger brother with CLN2 within months of each other. After discovering that a clinical trial was under way for Brineura, Dr. Wang fought to bring the new treatment to CHOC. By the time CHOC had been named an early access site for the new drug after a lengthy process, the older child had passed away.
“However, we had the opportunity to treat his younger brother before symptoms such as epilepsy really came to the fore,” says Dr. Wang. “It’s about finding avenues of hope for these families.”
CHOC takes a multidisciplinary approach to treating metabolic disorders to give patients the benefit of comprehensive expertise leading to the best outcomes possible, given their conditions.
“We have neurometabolic clinics in which various specialists can collaborate and see patients together,” Dr. Steenari says.
Providers and specialists involved in each patient’s care include Dr. Wang; Dr. Steenari; pediatric neurosurgeon Dr. Joffre Olaya, who administers every Brineura infusion; nurse practitioner Rebecca Sponberg; nurse manager Susan See; a nurse specially trained in these infusions; and a dietitian, social worker and case manager.
“This program is a great testament to the cooperation and collaboration between all of us on the team,” Dr. Wang says.
Many families of patients currently in the program travel long distances and have even moved to receive treatment at CHOC.
“When you offer something innovative and potentially curative, people are willing to travel across the country to seek it out,” Dr. Wang says.
The future of neurometabolics at CHOC
Since the inception of the program, the team at CHOC has administered more than 1,000 Brineura infusions, and they continue to refine the procedure.
“This is ongoing and open-ended, and the infusion devices have a finite lifetime,” Dr. Wang says. “They can only be accessed so many times before they need to be replaced, which means surgery. We also want to minimize the possibility of infection. This is a treatment going directly into the brain, so it is not without risk.”
The team is committed to making more advanced treatments available to patients. The next goal is to secure a clinical trial for gene therapy, which can allow a patient’s brain cells to make the enzyme on their own, eliminating the need for biweekly infusions.
To that end, Dr. Wang and the multidisciplinary neurometabolic team at CHOC have been selected for additional groundbreaking clinical trials of therapies for other neurodegenerative lysosomal storage disorders. CHOC was the first center selected out of four in the world for a first-in-human clinical trial of central nervous system gene therapy for a serious progressive condition called mucopolysaccharidosis type I, also known as Hurler Syndrome; to date, the team at CHOC has administered the gene therapy to 66% of all children treated — including children from West Virginia, Vermont and Tennessee.
Thanks to the team’s expertise in central nervous system gene therapy, CHOC was selected for another first-in-human clinical trial of central nervous system gene therapy for GM1 gangliosidosis. Collaborating with centers from Manchester, UK and Paris, Dr. Wang’s team treated a young child from Missouri, becoming the second hospital in the world to administer the investigational medication that could be a one-time therapy for the condition.
“The neuro-lysosomal team knows the love that parents have for their children, as well as the heartbreak and anguish that come with the diagnosis of a pediatric inherited neurodegenerative condition,” Dr. Wang says. “We have a very knowledgeable, experienced team of specialists who don’t like to say, ‘There’s nothing we can do.’ We are committed to providing hope to families in the form of access to clinical trials of potential therapies for their children.”
Learn more about the Neurometabolic Program at CHOC.

CHOC Hospital was named one of the nation’s best children’s hospitals by U.S. News & World Report in its 2025-26 Best Children’s Hospitals rankings and ranked in the neurology/neurosurgery specialty.