The most common complication experienced among preterm neonates—bronchopulmonary dysplasia (BPD)—is associated with long-term health issues, increased healthcare burden and cost, parental anxiety and hospital readmission. Previous research has sought to both understand and reduce BPD. While preventing BPD has been deemed challenging, a careful evaluation and update of intervention protocols at CHOC has produced a distinct reduction in chronic lung disease (CLD) in preterm infants.
“Based on the literature and after consulting experts across the country, we believe some babies will develop BPD based on environmental or genetic factors that are beyond our control as neonatologists,” says Dr. Michel Mikhael, medical director of Small Baby Unit at CHOC and assistant professor of clinical pediatrics at the University of California, Irvine School of Medicine. “Even when applying evidence-based medicine, it is difficult to reduce severe BPD in some infants. We focus on what we can do when patients come to us, applying evidence-based medicine to help patients achieve their maximum potential.”

To that end, the CHOC Small Baby Unit multidisciplinary team recently reviewed three years of baseline data and found multiple areas for improvement within its BPD intervention protocols. The team then developed these focus areas into an interdisciplinary quality improvement program to reduce chronic lung disease in preterm neonates.
Taking the SMART approach
The following five factors were pinpointed as potential drivers of change and targeted as SMART aims:
- Improved compliance with “Golden Hour” goals of care
- Timely administration of surfactant for infants with respiratory distress syndrome (RDS)
- Optimized noninvasive ventilation and introduced less invasive surfactant administration (LISA)
- Standardized steroid administration for evolving BPD to a proactive risk-stratified approach
- Standardized respiratory care (ventilator and CPAP guidelines and oxygen challenge test)
CHOC began offering a procedure not commonly performed in the United States, despite being a gold standard for BPD prevention in Europe. Known as LISA (less invasive surfactant administration), the procedure involves placing a thin catheter beneath the vocal cords to administer surfactant into the lungs, while infants spontaneously breathe. This allows the natural distribution of surfactants and decreases mechanical ventilation exposure, which is the highest risk factor for BPD development. The CHOC team developed an educational video to facilitate this new procedure rollout and has been sharing it with other neonatal units.
To ensure adherence to the five key drivers, education was provided to all who interact with patients. Additionally, bedside decision-aid tools were developed to help guide CHOC’s team of multidisciplinary providers.
Early results show significant promise
Since the implementation of this project, the CHOC team has noted a marked reduction in CLD. Those admitted to CHOC within the first day of life experienced the greatest improvement, with CLD rates dropping from 38% to 19%.
“We have improved the delivery of evidence-based practices and saw an improvement with the outcome as a result” Dr. Mikhael says.
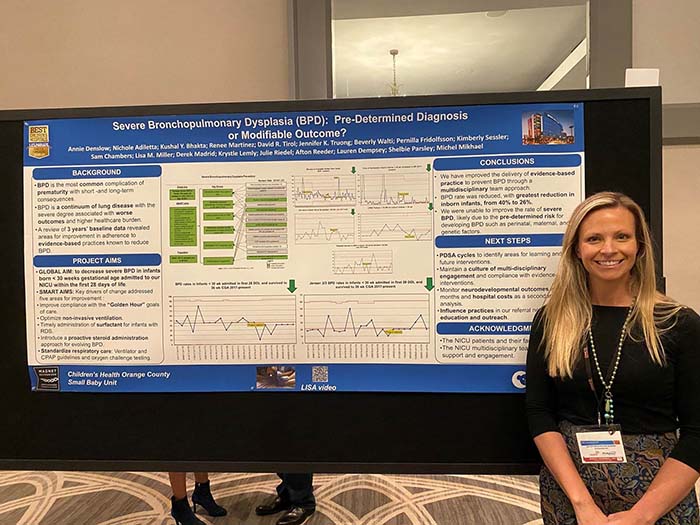
Other improvements implemented include:
- “Golden Hour” care provided approximately 40 minutes faster than before
- Decreased CPAP failure, reduced by one-third (now approximately 20%)
- Time to surfactant administration reduced from 120 minutes to less than 30 minutes
Another positive trend is the overall reduction of BPD cases coming to CHOC. This is due to CHOC’s aggressive education efforts within its neonatology referral network. As these referral hospitals implement CHOC guidelines, neonatal patients with BPD can receive evidence-based care close to home, reducing stress on families.
Looking toward the future of BPD care
Encouraged by these positive results, CHOC neonatologists plan to continually improve their care of neonates experiencing BPD. The immediate next steps include implementing video recording of delivery room resuscitation and introducing volume guarantee ventilation.
Researchers also aim to safely bridge the gap between the NICU and an outpatient environment. To meet this goal, neonatologists will work with pulmonologists, social workers, nutritionists and other professionals.
Future research should uncover new therapies for this common condition.
“Stem cell and microbiome lung research in this area may be very helpful,” Dr. Mikhael says. “I anticipate great benefit to identifying children who should be screened early based on genetic predispositions and providing individualized, targeted therapies.”
CHOC was named one of the nation’s best children’s hospitals for neonatology by U.S. News & World Report in its 2025-26 Best Children’s Hospitals rankings.




