CHOC participates in research study to improve sepsis treatment in kids
Over the past several decades, improvements have been made in the outcomes of patients with sepsis, an infection of the blood stream that can lead to organ failure and death.
But treatment for these critically ill patients has remained the same: Give them fluids and antibiotics and other forms of supportive care, and hope for the best.
Research over the last two decades, however, has shown that there are dramatic variations in the way a child’s immune systems respond to sepsis.
Could treatment and therapies be designed to address each patient’s immune profile?
That’s the critical question doctors at CHOC, in collaboration with 23 other leading U.S. pediatric healthcare systems, are working on answering.
Moving the needle in the diagnosis and treatment of sepsis in children
Taking small samples of blood from children whose sepsis has led to the failure of at least two major organs, researchers are studying whether targeted immunomodulation could result in better recovery and survival rates.
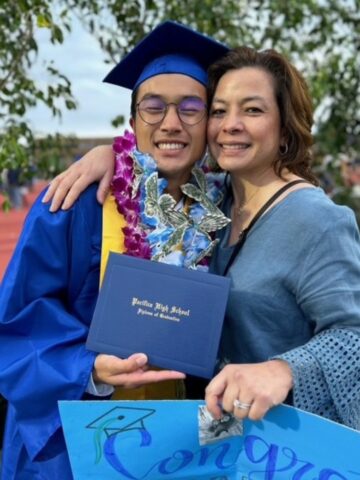
“What we’re doing in trying to move the needle in the diagnosis and treatment of sepsis is really exciting,” says CHOC pediatric critical care specialist Dr. Adam Schwarz.

In a nod to its growing reputation as a provider of excellent and innovative pediatric critical care, CHOC recently was welcomed into an invite-only research consortium of the nation’s top children’s hospitals, CPCCRN, for Collaborative Pediatric Critical Care Research Network.
Now, the collaborative is two years into a study that, by spring 2026, could lead to better outcomes in children with sepsis-induced multi-organ dysfunction syndrome (MODS) by delivering medications that best work with how their immune system is responding to their blood-stream infection.
“The thinking is,” explains Dr. Schwarz, “not everyone responds the same way to being infected. There are different subtypes, or phenotypes, for sepsis, meaning one population of patients responds one way, and another population of patients another way.
“What if we could test for that? What if we could determine what ‘flavor’ of sepsis they have, then use immunotherapy to modify their response to sepsis to see if we could get quicker or better survival outcomes or recovery from organ failure?”
The result, Dr. Schwarz adds, could save lives.
Overnight delivery of blood samples for sepsis research studies
So far, 13 CHOC patients have been enrolled in the study, PRECISE, for Personalized Immunomodulation in Pediatric Sepsis-Induced MODS.
Researchers hope to enroll 1,000 patients from newborns to 17-year-olds at the 24 pediatric hospitals in the CPCCRN network, says Dr. Mark Hall, the principal investigator of the PRECISE study and chief of the Division of Critical Care Medicine at Nationwide Children’s Hospital in Columbus, OH.
“These patients might end up benefiting from different therapies based on their immune profiles,” Dr. Hall says.
CHOC and other hospitals participating in the PRECISE study obtain blood samples from enrolled subjects, process them locally, freeze them, and then ship them overnight to Nationwide Children’s Hospital for analysis by Hall and his team of researchers.
Based on test results, the study participants are placed into one of several different cohorts based on the severity of inflammation they are experiencing and whether their white blood cells are underactive (immunosuppressed) or normal. Some children might receive an immunostimulatory medication (or placebo), while others might receive an anti-inflammatory medication (or placebo). Still others might simply be observed without any immunomodulatory medication at all.
The medications being used in the PRECISE study are both already approved by the Food and Drug Administration for other conditions.
“CHOC and Dr. Schwarz and his researcher coordinator staff have been outstanding partners in the conduct of this study,” Dr. Hall says.
First study of its kind
Dr. Schwarz, who supervises the clinical research program within CHOC’s division of pediatric critical care notes that to participate in the study, patients have to be extremely ill.
“It’s a very complex trial,” he says. “Patients have to be sick enough in an intensive care unit with two or more major organ failures persisting into a third day.”
He says the seven CHOC patients who have participated in the study thus far all got better.
“But we’re blinded to the treatment,” he says of the study’s clinical trials. “We don’t know if their recovery was expedited by our study drugs or not.
“Regardless,” Dr. Schwarz adds, “this is the first targeted immunomodulation study of its kind for the treatment of organ-system failures in patients experiencing septic shock. If this pans out, this will mark the first time in which phenotype testing has been performed and treatment has been targeted based on how a patient is responding to sepsis.”
Learn about pediatric research and clinical trials at CHOC