Leukemia is the most prevalent childhood cancer, affecting one-third of all children and adolescents who develop cancer. Of those patients, three-fourths are diagnosed with acute lymphoblastic leukemia (ALL), the most common type of pediatric leukemia. ALL currently has a mean five-year survival rate of 90%. However, that rate is lower in certain demographics and for certain subtypes of the disease.
Physicians at Children’s Hospital of Orange County (CHOC) are committed to improving survival rates for all patients with pediatric leukemia. They are also exploring how to mitigate the toxicity of specific treatments, which can prevent patients from taking medications that are more likely to eliminate the cancer.
“One of my biggest interests is chemotherapy toxicities and disparities in outcomes, especially related to which ethnic groups have those disparities, why they occur and how we can overcome those disparities,” says Dr. Van T. Huynh, oncologist, director of CHOC’s Leukemia Program and section director of the CAR T-cell/Immunotherapy Program.
Ameliorating asparaginase response and related disparities
ALL is more common in Hispanic and white children than in Black or Asian children, which makes CHOC an ideal site for research into toxicity and outcomes disparities.
“Around 50% to 60% of our ALL patients are Hispanic, and what I’ve noticed through the years is that the toxicity they experience is more profound than in non-Hispanic patients,” Dr. Huynh says. “They also seem to have worse outcomes overall.”

Dr. Huynh is leading a multicenter study investigating response to pegaspargase, a chemotherapy that is essential in pediatric ALL treatment regimens. Asparaginase therapy has significantly improved patient survival, but it has several side effects, including clinical hypersensitivity among children with ALL. Thus, patients with hypersensitivity reactions must switch treatment and receive an alternative formulation that is shorter acting and requires six doses for one dose of pegasparagase. This isn’t ideal and can be more painful when given intramuscularly, and the multiple doses are often inconvenient for patients.
“The goal of this study is to determine whether premedication with a histamine-1 and histamine-2 blocker can alleviate hypersensitivity and avoid the need to switch to an alternative therapy,” Dr. Huynh says.
Therapeutic drug monitoring is also performed to distinguish between true hypersensitivity versus infusion reactions. A subset of patients with hypersensitivity are also re-challenged to pegaspargase through desensitization.
“Additionally, since we observe a high incidence of other severe toxicities in our Hispanic population from asparaginase therapy, we are also interested in understanding whether factors such as ethnicity, obesity, sex or age increase their risk,” Dr. Huynh says.
The study will also involve sequencing patients’ genes to determine the single nucleotide polymorphisms (SNPs) that may be driving the differences in asparaginase hypersensitivity and toxicity.
“I hope this study could be a game changer for treating patients (with ALL) by identifying ways to decrease the incidence of hypersensitivity and understanding those who are most at risk for certain toxicities associated with asparaginase,” Dr. Huynh says.
Combining therapies in hopes of improved survival rates
One subtype of ALL, Philadelphia chromosome-like (Ph-like) ALL, occurs in about 15% of pediatric patients and in about 27% of adolescent young adults. Compared with the five-year 90% survival rate of standard ALL, Ph-like ALL has a poor five-year survival rate of only 63%. For reasons not well understood, Hispanic patients have the highest incidence of Ph-like ALL.
Dr. Huynh’s new study, in partnership with Dr. David Fruman at the University of California, Irvine, examines whether adding tyrosine kinase inhibitors (TKI) to standard chemotherapy improves overall survival rates for patients with Ph-like ALL. In addition, Dr. Huynh and Dr. Fruman are investigating whether patients whose cancer has a CRLF2 fusion could respond to standard chemotherapy and TKI combined with a third-generation bi-steric mTOR inhibitor.
“We know that the mTOR is a kinase,” Dr. Huynh says. “It integrates signals from growth factors in the environment and it regulates cell growth, metabolism and proliferation survival.”
Preclinical studies have found the bi-steric mTOR inhibitor has activity in leukemia cells.
“Our research is taking this one step further by utilizing this novel combination of therapy. We’re sampling bone marrow from newly diagnosed Ph-like ALL patients and producing xenograft models in mice to test the efficacy of the combination,” Dr. Huynh says. “Ultimately, we’re hoping we can show this combination is effective for Ph-like ALL and develop a phase 1 clinical trial for patients.”
One acute lymphoblastic leukemia patient, multiple studies
Dr. Huynh and the CHOC oncology team participate in multiple clinical trials through the Children’s Oncology Group (COG), including Project:EveryChild, which maintains a childhood cancer registry and biorepository for every patient at CHOC and around the country. One patient whose tissue is on file, Liliana, was first diagnosed with B-cell ALL as a teenager.
“Her initial therapy was complicated by toxicity from chemotherapy and steroids,” Dr. Huynh says. “She had an extremely difficult time.”
However, Liliana benefited from a COG phase 3 clinical trial involving inotuzumab treatment.
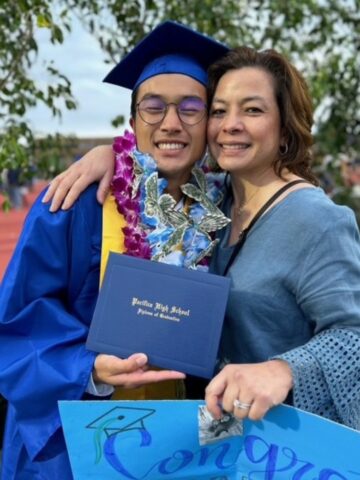
“She is now a young adult who has completed therapy and graduated from college. Liliana has done wonderfully,” Dr. Huynh says. “She is a part of our cancer survivorship clinic now and also serves as a mentor to other patients. She has come back to share with other young adults what she’s learned and what she’s gone through.”
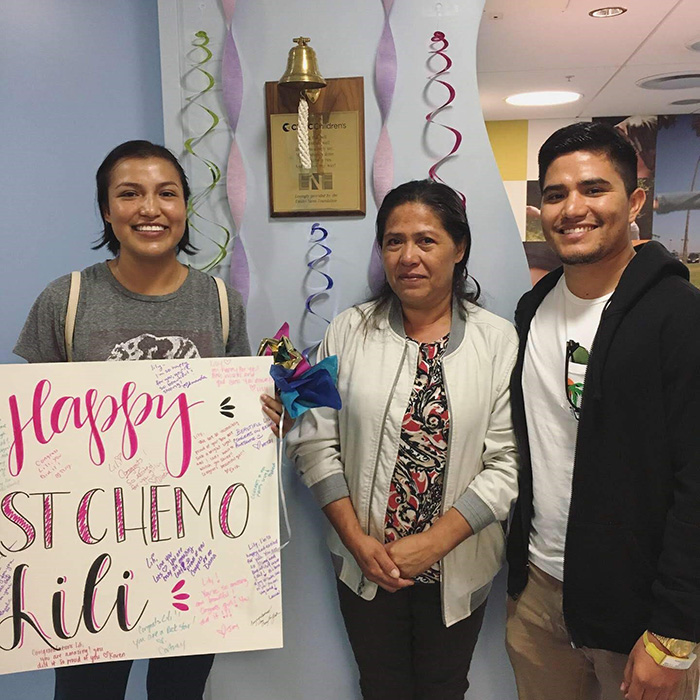
Liliana has also participated in a COG specimen procurement trial, in which her blood and bone marrow biopsies were collected at diagnosis, during therapy and after treatment as part of ongoing immunophenotyping for ALL confirmation and classification. She also participated in a study assessing the helpfulness of Voicing My CHOiCES as a tool for advanced care planning.
Liliana also contributed to the ongoing Reducing Ethnic Disparities in Acute Leukemia (REDIAL) Consortium. CHOC is the only pediatric cancer center outside of Texas invited to join the consortium, which is led by Texas Children’s Hospital.
“Because we have such a large Hispanic patient population, and this population has high toxicity and low survival, REDIAL hopes to find answers as to whether there are any environmental impacts that lead to the development of acute leukemia,” Dr. Huynh says. “With several thousand patients enrolled, it’s one of the largest studies underway looking at the epidemiology of childhood cancer. Ultimately, the consortium hopes to have a better understanding so we can change treatment options to minimize toxicity and improve survival rates.”

CHOC will continue providing advanced care and access to clinical trials to ensure the best possible outcomes for all patients.
“The wonderful thing about CHOC is not only do we offer a high level of comprehensive care and unique clinical trials, but we also have an amazing team of providers who are compassionate and work with patients to address all aspects of their complex care, including psychosocial, psychological, financial and support for families,” Dr. Huynh says.

CHOC Hospital was named one of the nation’s best children’s hospitals by U.S. News & World Report in its 2025-26 Best Children’s Hospitals rankings and ranked in the cancer specialty.