Promoting novel brain tumor treatments at CHOC
Dr. John Crawford shares a pediatric neurologist’s perspective on how neuroscience and oncology can come together to advance the treatment of pediatric brain tumors. Read pediatric oncologist Dr. Mariko Sato’s perspective here.
A collaborative endeavor of providers in the neuroscience and oncology programs at Children’s Hospital of Orange County (CHOC) brings a unique multidisciplinary approach to the treatment of pediatric brain and spine tumors – and has already sparked new research studies.
The collaboration of the Hyundai Cancer Institute at CHOC and the CHOC Neuroscience Institute has long set the Brain and Spine Tumors Program apart with novel diagnostic approaches and complementary treatment options. Yet the recent alignment between pediatric neurology, neurosurgery and oncology allows CHOC providers to explore multifaceted treatments using a wider range of technologies and expertise.


The collaboration is led by Dr. John Crawford, division chief of child neurology and neuro-oncologist at CHOC and co-medical director of the CHOC Neuroscience Institute, and Dr. Mariko Sato, pediatric neuro-oncologist and director of the Brain and Spine Tumors Program at CHOC. As newcomers to CHOC, Dr. Crawford and Dr. Sato hope to bring together the best parts of their training and experiences at different institutions to increase the strength and scope of CHOC’s clinical care and research capabilities.
“My role in the neurology department at CHOC is what I would describe as a laser-focused ‘matchmaker,’ because you’re pulling in different disciplines to diagnose and treat one disorder,” Dr. Crawford says. “We’re treating these tumors by utilizing a specific subset of very talented individuals focused on targeting a single disease.”
An alliance that generates new research
Since the closer alignment among specialists began in spring 2022, collaborators already have several research and clinical trials under way:
- A multidisciplinary tumor board performs genomic analysis to customize tailored treatments based on the patient’s genetic mutations, to be studied prospectively.
- A multi-institutional vaccine trial for childhood diffuse intrinsic pontine glioma is in process at CHOC and University of California, Irvine.
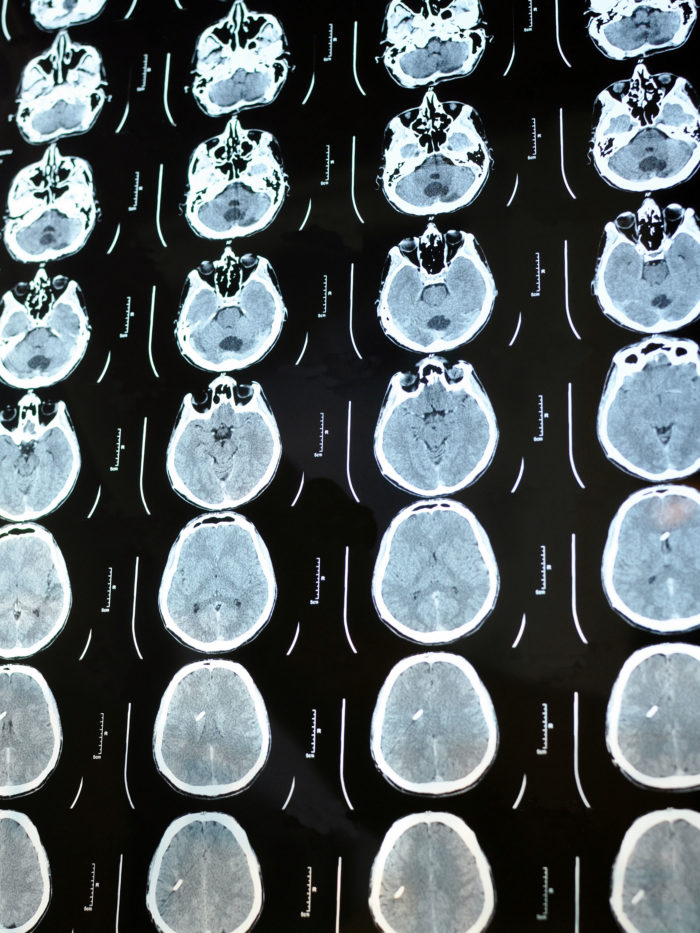
- Dr. Crawford’s recent paper in Frontiers in Oncology entitled “Characterization of pediatric brain tumors using pre-diagnostic neuroimaging” introduces one of the first steps in attempting to understand the genesis of a brain tumor.
“I reviewed over a thousand patients with brain tumor diagnoses who had imaging prior to their diagnosis — such as scans for prior concussions, head injuries, headaches or other indications,” Dr. Crawford says. “I’m interested in whether we can use these images to understand the genesis of brain tumors because patients and families want to know how long that tumor has been inside that brain. That’s a very logical question that I’ve been asked for the last 20 years. By analyzing these neuroimages, I want to answer that question in a statistically meaningful manner.”
Combining pediatric neurology and neurosurgery with neuro-oncology to target tumor treatments
As well as inspiring new research, the collaboration enables physicians to deploy existing technologies to their fullest potential. This includes advances in targeted radiation in the radiation oncology program. CHOC’s neurosurgeons also collaborate with neuro-oncologists to use laser interstitial thermal therapy to pinpoint and treat a subset of difficult-to-access tumors.
Additionally, the physicians in the collaborative program use robotically guided technologies to take minuscule core biopsies from selected samples in the brain that are otherwise difficult to access. Physicians have subsequently used that tissue for molecular genetic technologies to aid in tumor diagnostics.
“What’s most exciting about the use of these technologies is their ability to provide novel therapies for patients,” Dr. Crawford says. “We can provide true individualized care; we’re no longer treating patients using recipes based on the name of a tumor or what it looks like under the microscope. We’re tailoring these treatment plans to the exact genetic underpinnings of the patient’s tumor.”
Improving patient care through a whole-patient approach to treatment
The ongoing collaboration also allows physicians and supporting providers to treat the “whole patient.” For Dr. Crawford, this means viewing disease and patient not as parallel but as overlapping pathways, an approach other institutions could adopt.
“We don’t treat the disease without having the patient’s best interest in mind,” Dr. Crawford says. “That really pertains to side effects of therapy, as well as its short and long-term effects, which could be anything from headaches and vision changes to neurocognitive and behavioral sequelae and their effect on the mental health of the patient. While we want positive outcomes and disease cures, curing a patient when the patient isn’t free of neurologic deficits is a failure in our minds.”
Looking to a bright future
The pediatric neurology, neurosurgery and oncology collaboration builds on a tradition of cross-collaborative efforts that have defined patient care at CHOC.
“We are willing to think outside of the box when it comes to treating childhood cancer,” Dr. Crawford says. “Our neuroscience community is best served with collaboration throughout the state and nationwide. CHOC is one large program on the map, and I look forward to cross-institutional collaboration from California and beyond.”

CHOC Hospital was named one of the nation’s best children’s hospitals by U.S. News & World Report in its 2025-26 Best Children’s Hospitals rankings and ranked in the neurology/neurosurgery specialty.