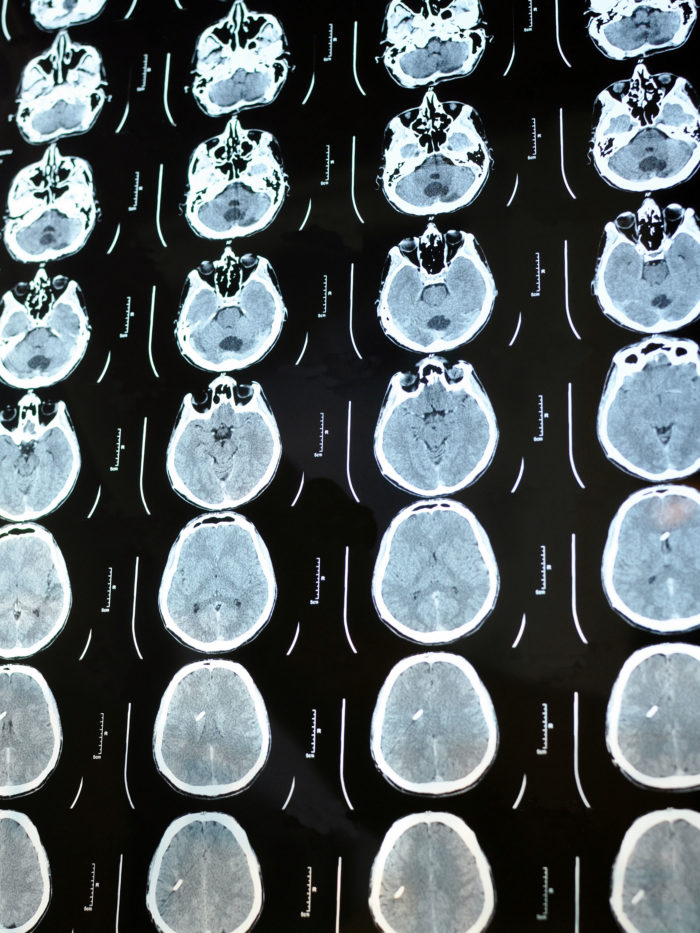
Combining expertise to optimize outcomes for pediatric brain and spine tumors
Dr. Mariko Sato shares a pediatric oncologist’s perspective on how oncology and neuroscience can come together to advance the treatment of pediatric brain tumors. Read pediatric neurologist Dr. John Crawford’s perspective here.
The Brain and Spine Tumors Program at the Hyundai Cancer Institute at Children’s Hospital of Orange County (CHOC) represents a growing alignment between specialists in neurosurgery, neurology and oncology to provide collaborative, integrative diagnosis, evaluation, treatment, follow-up and post-treatment rehabilitation for kids and young adults with brain and spine tumors.
Dr. Mariko Sato, pediatric neuro-oncologist and director of the Brain and Spine Tumors Program at CHOC, leads the multidisciplinary team alongside Dr. John Crawford, division chief of child neurology at CHOC and co-medical director of the CHOC Neuroscience Institute. As newcomers to CHOC, Drs. Sato and Crawford hope to bring together the best parts of their training and experiences from previous institutions to increase the strength and scope of CHOC’s clinical care and research capabilities.


“Dr. Crawford and I come in with a pretty similar perspective about treating pediatric brain tumors,” Dr. Sato says. “In terms of voicing changes and sharing insights to facilitate collaboration across many subspecialties, two is better than one.”
The unique contributions of each member of the diverse group of specialists enhance CHOC’s efforts to optimize outcomes and quality of life for pediatric patients and their families.
“By combining everybody’s expertise, we are better able to make the right decisions for patients,” Dr. Sato says. “I consider this program as being like an orchestra — everybody has a part.”
Keeping pace with a rapidly changing field
While an increasingly precise understanding of pediatric brain and spine tumors and growing availability of novel treatment options has opened a new range of possibilities for patients, these developments have also vastly complicated the process of diagnosis and treatment planning. Diversification in treatment approaches is driven in part by advances in tumor pathology, such as the molecular stratification of tumors into distinct subgroups. Increased recognition of genetic factors that influence tumor formation also informs decision-making.
“The brain tumor field is really changing,” Dr. Sato says. “For example, where we used to have one treatment for a medulloblastoma, which is the most common brain cancer, we now have to consider up to 12 risk stratifications to treat this cancer.”
According to Dr. Sato, coordinating closely with specialists in fields other than oncology is vital to eliminate the tumor in a timely fashion, while mitigating the aftereffects of treatment itself.
An alliance that generates new research
Since the closer alignment among specialists began in spring 2022, collaborators already have several research and clinical trials under way:
- A multidisciplinary tumor board performs genomic analysis to customize tailored treatments based on the patient’s genetic mutations, to be studied prospectively.
- We focus on enrolling patients to active clinical trials. By doing so, both physicians and patients can contribute to the progress of science, to achieve better outcomes of pediatric brain and spine tumors.
- A multi-institutional vaccine trial for childhood diffuse intrinsic pontine glioma is available now at CHOC.
- Collaboration with UCI labs lead by Dr. Daniela Bota, we are developing patient derived tissue culture and xenograft models as a future research equipment.
Meeting each patient’s unique needs
When a patient presents with symptoms that suggest any type of brain or spine lesion, specialists from neurosurgery, neurology and oncology now meet to discuss the case from the beginning. These initial consultations help guide diagnosis and outline a treatment plan, which usually begins with neurosurgery.
“I try to meet the patient before the surgery and, when I have the chance, go into the operating room,” Dr. Sato says. “This is so the oncology team can contribute to surgery as much as possible. We can also observe the tumor during surgery and see if we can maximize the research opportunity using patient tissue with patient consent.”
Once the team has completed a pathology study and made a diagnosis, a tumor board reviews each patient’s case. The tumor board continues to meet regularly to discuss treatment options and monitor patient progress.
“Every single case involves difficult-to-make decisions,” Dr. Sato says. “We always discuss these cases at the tumor board, at the right timing so that everybody sees the new patients and then agrees on the management. Our team approach allows us to see things from different angles and personalize recommendations for each patient.”
Building a foundation for the future
The alignment of this multidisciplinary team demonstrates CHOC’s commitment to providing optimal clinical care for pediatric patients. The team is expansive, including neuro-radiology, neuro-pathology, radiation oncology, ophthalmology, endocrinology, neuropsychology, palliative care, rehabilitation, nutritionists, child life and social work. CHOC also plans to include neuro-oncology researchers to develop new therapies along with learning from patients.
Further plans for program expansion include developing more partnerships with institutions outside of CHOC, providing patients with greater access to clinical trials and advanced treatments such as proton beam radiation therapy. Dr. Sato also hopes to develop a neuro-oncology fellowship program to train the next generation of specialists and researchers.
“We cannot focus on clinical practice exclusively,” Dr. Sato says. “We also need to contribute to translational research to answer questions that came from our patients. Unfortunately, not everyone with brain and spine tumors has good outcomes. I believe that our research efforts will change some of the outcomes for these patients in the future.”
Learn more about the multidisciplinary Brain and Spine Tumors Program at CHOC

CHOC Hospital was named one of the nation’s best children’s hospitals by U.S. News & World Report in its 2025-26 Best Children’s Hospitals rankings and ranked in the cancer specialty.