CHOC has emerged as a leader in implementing a new global standard for assessing food and liquid consistencies for patients with swallowing difficulties.
CHOC was one of the first pediatric hospitals nationwide to implement the International Dysphagia Diet Standardization Initiative (IDDSI), which aims to establish a standardized system of measuring and labeling the thickness of food and drink.
The goal is to ensure patient safety and improve treatment outcomes, say Jennifer Raminick and Danielle Monica, two CHOC speech language pathologists who spearheaded the system’s adoption.
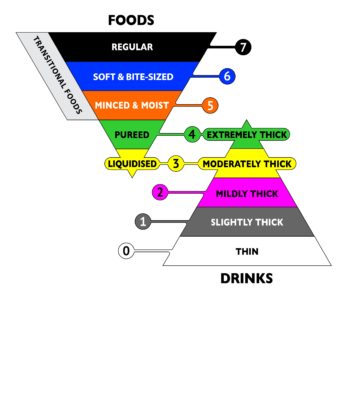
Established in 2013 by a group of dysphagia specialists, IDDSI was created to standardize descriptions, consistencies and terminology for diet modifications for patients of all ages, locations and cultures.
The initiative is a marked departure from previous guidelines that relied on ambiguous labels and descriptions that often varied across institutions and providers, and required specialized, arcane equipment to measure food consistency.
(c) The International Dysphasia Diet Standardisation Initiative 2016 @http://iddsi.org/framework/.
Conversely, IDDSI guidelines are simple and clear; testing is easy and takes 10 seconds or less; and testing tools are easily accessible to providers and at-home caregivers, Danielle and Jennifer say.
Here’s a brief explanation of the flow testing process to assess a liquid’s thickness: Cover the spout of a 10-mL syringe and fill it with the liquid. With a stopwatch in hand, open the spout for 10 seconds, and then stop the flow. The amount of substance remaining in the syringe is then compared to a rubric to gauge its consistency.
If 1 to 4 mL of the substance remains in the syringe, it is considered of “slightly thick”; 4 to 8 mL remaining is considered “mildly thick”; 8 to 10 mL is “moderately thick” or liquidized; and a substance with 10 mL remaining is “extremely thick” or pureed.
Beyond those categories, food is assessed and labeled as, “liquidized” “pureed” “minced and moist,” “soft and bite-sized” or “regular.” These categories are determined by how the food flows off a spoon or fork, or by measuring a food particle against a ruler.
To implement the program house-wide, the rehabilitation services team partnered with several other departments and disciplines.
Jennifer and Danielle worked with CHOC’s Clinical Nutrition and Lactation department as well as the food service team to create a specific menu for dysphagia patients. It included limited options for each level of consistency and easy-to-follow recipes with three ingredients or less. All food is made from scratch.
The rehabilitation services team developed curriculum for multi-level education of current and new dysphagia therapists, physicians, nursing, dietitians, and food service staff members.
Learn more about rehabilitation services at CHOC.




