A bout with an optic glioma as a toddler didn’t keep Dr. Sonia Morales from making the most of her childhood and adolescence, and working toward a future career as a pediatric oncologist.
But as a young adult in medical school with reason to learn more about her childhood illness, Dr. Morales realized just how little she herself knew about her diagnosis, treatment and her roadmap for life post recovery.
She also learned that while her parents spoke glowingly of her care team and could recite the timeline of her treatment, finer details like her exact diagnosis and other medical jargon were missing from their memory. Or, more likely, as native Spanish speakers, her parents were never made fully clear of their daughter’s case.

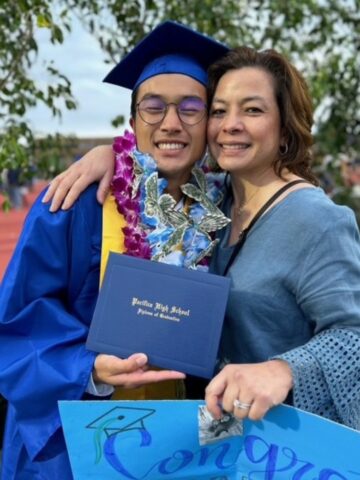
“My parents were able to advocate for me as best they could,” says Dr. Morales, who just joined the Hyundai Cancer Institute at CHOC after completing her fellowship there earlier this fall. “I don’t know if it was a language piece. Medical lingo doesn’t always translate well.”
So, all that considered, it’s no surprise that Dr. Morales would be passionate about patients and families fully understanding their diagnoses, treatment plan and survivorship roadmap, as well as working to establish more trust of medical institutions, healthcare providers and medical research among people of color.
Joining a prestigious group
Dr. Morales is among the inaugural cohort of physicians to be trained in the Bristol Myers Squibb (BMS) Foundation Diversity in Clinical Trials Career Development Program, in partnership with the National Medical Fellowships (NMF) and the American Association for Cancer Research (AACR).
Fifty-two physicians from across the United States were selected for the five-year, $100 million initiative that is part of the BMS Foundation’s commitment to health equity, diversity and inclusion.
Chosen by an independent selection committee, Dr. Morales and her cohort are an accomplished group working at a broad range of healthcare institutions in 22 states across the U.S. Dr. Morales is one of five from California.
Thirty-four women and 18 men who represent a diverse cross section of races and ethnicities, the physicians bring a widely varied perspective and range of experiences to the program, as well as to their therapeutic focus areas of cancer (hematologic or solid tumors), immunologic disorders and cardiovascular diseases.
With data showing that nearly 80% of patients participating in clinical trials are white, the Diversity in Clinical Trials Career Development Program was launched to address the lack of diversity in clinical trials in the U.S.
Dr. Morales and her peers will be trained as world-class clinical research scientists with additional knowledge, skills and competencies in effective community outreach and engagement. According to BMS, this new generation of physician investigators will have the potential to transform the clinical research landscape by conducting clinical trials designed with the goal of increasing the diversity of their participants.
The multi-dimensional program is uniquely designed to foster clinical and translational research that is community-informed, designed and conducted.
Participants receive training in evidence-based methods of community outreach and engagement. They participate in a multi-level mentorship model with established community-based Principal Investigators and with medical students through a major component of the program called the Clinical Investigator Pipeline Program (CIPP).
The CIPP is an intensive summer service-learning externship that exposes promising rising second-year medical students who are underrepresented in medicine to the basics of clinical trials and to working in underserved community health settings to provide outreach, education and engagement on clinical trials.
“I’m a strong believer in pipeline programs – I was part of them all throughout my undergraduate career and I’m still part of pipeline programs,” Dr. Morales says. “I think what helped me get into research was meeting a pediatric oncologist who was doing research on cancer survivorship, specifically disparities in Latino communities. That inspired me to get my master’s degree in public health, and that’s one of the reasons that I joined this program. I want to bring more diversity into clinical programs.”
A science career sparked by literature
An avid reader as a child, Dr. Morales was captivated by a novel in which a teenaged character was diagnosed with leukemia. Using a dial-up modem, she searched online for more information about the condition and came across Camp Ronald McDonald for Good Times, a program that provides residential camping experiences for children with cancer. Dr. Morales waited patiently until she was 18 and then applied to become a camp counselor.
From there, the interest continued to root and she pursued her passion as an undergraduate student at UCLA. There, Dr. Morales met one of her mentors who was doing survivorship research and needed someone to transcribe interviews.
Dr. Morales went on to earn her medical degree from the Program In Medical Education (PRIME) at the Charles Drew University School of Medicine and Science/ David Geffen School of Medicine. While in medical school, she received her master’s degree in public health, with an emphasis in health policy and management from the Fielding School of Public Health at UCLA.
From there, Dr. Morales completed her chief residency and pediatrics training at Harbor-UCLA Medical Center. She’s also held various leadership positions within the Latino Medical Student Association and the National Hispanic Medical Association.
Throughout her three-year hematology/oncology fellowship at CHOC and now as a member of junior faculty, Dr. Morales’ passion has translated into the care of children, teens and young adults at the Hyundai Cancer Institute.
The aim of Dr. Morales’ current research project is to develop an app that can be used as a mental health intervention for cancer survivors.
The project builds upon the research of Dr. Lilibeth Torno, a CHOC oncologist who is investigating the barriers that cancer survivors have to receiving survivorship care.
In looking at Dr. Torno’s preliminary data, Dr. Morales and colleagues have gleaned that cancer survivors would appreciate a mental health component to survivorship care. The app then would allow survivors to send real-time mood data to clinicians, who could then connect them with community services, if needed.
Dr. Morales sees other possibilities for the app, as well.
“Our hope would be to develop an intervention that could be used in other populations– not just cancer survivorship,” she says. “We’re seeing now with COVID, the extent that mental health has been affected, even with younger children.”
Learn about pediatric research and clinical trials at CHOC