CHOC metabolic disorders division has discovered a previously unreported condition that could provide answers for parents of children experiencing unexplained liver failure.
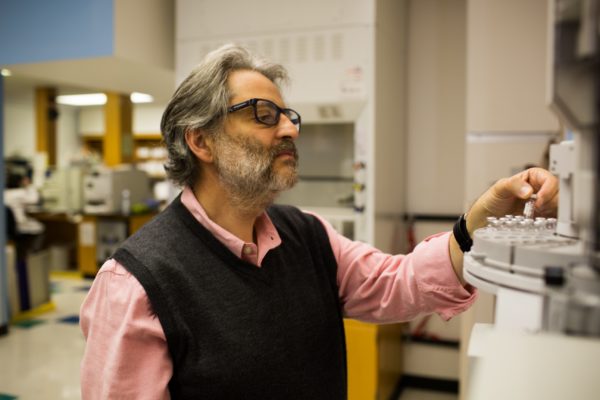
Led by Dr. Jose Abdenur, the division’s medical director, the team has coined the genetic condition Mitochondrial Transcription Factor A (TFAM) deficiency and has published its findings this month in the journal Molecular Genetics and Metabolism.
The condition affects mitochondria, the energy-producing part of cells. If this transcription factor, a protein that binds to mitochondrial DNA, isn’t working, the body cannot maintain its mitochondrial DNA, which is essential to creating energy.
The infant patient described in the paper died from liver failure as a result from the mitochondrial DNA depletion. Subsequent testing concluded that her older brother also died previously from the same cause at 2 months of age.
Patient history
The 12-week-old patient presented at CHOC in 2015 after her newborn screening detected elevated levels of tyrosine, an abnormality that may indicate liver disease.
Blood tests revealed elevated liver enzymes, abnormal bilirubin levels and low blood sugar levels. She was soon diagnosed with cirrhosis.
CHOC worked with UCLA to perform whole exome sequencing of the patient. The laboratory found two mutations on TFAM, a gene that had never previously been associated with human disease. However, previous studies had shown that a mouse model with mutations in this gene developed lethal mitochondrial depletion. This information was a clue to pursue research studies at CHOC’s laboratory in the patient’s fibroblasts for energy metabolism, which proved the pathogenicity of the mutation.
Additional molecular testing found the same homozygous variants in blood samples from the deceased sibling. While this genetic work was underway and about 10 days after the baby’s original admission to CHOC, the patient’s condition deteriorated further.
The team deemed the patient an unsuitable transplant candidate due to her condition being multisystemic. Because her liver had deteriorated so significantly and her muscles were also becoming affected, her family, in agreement with clinicians, opted not to pursue further heroic measures. They received palliative support care and the baby died at about 4 months old.
Future impact
Though this discovery will not bring back their children, the family is grateful to CHOC for providing answers and is hopeful that the discovery will lead to early diagnosis and treatment of this condition in other infants.
Dr. Abdenur expects the discovery and publication will lead liver centers to look at their samples for mitochondrial defects. CHOC’s team will also continue to work on the cells to potentially develop an experimental treatment in the future.
The full paper can be read in the journal Molecular Genetics and Metabolism.




