Data shows that CHOC intensive outpatient program (IOP) for high school teens is successfully intervening on suicidal behaviors in participants.
Clinicians examined self-reported data gathered from patients and their parents since the launch of CHOC’s IOP in March 2018. Participants reportedly experienced less distress after completing the program, a sentiment echoed by their parents. Further, the specific sets of behaviors treated by the IOP (e.g., suicidality, emotion dysregulation and impulsivity) demonstrated reliable improvement.
“It is incredibly rewarding that our patients and their parents are experiencing meaningful improvements from CHOC’s intensive outpatient program,” says Dr. Micaela Thordarson, the program’s lead psychologist. “This data shows that we are effectively reducing stress and high-risk behaviors in our patients, which is part of the mission we set when developing and launching the IOP.”
How CHOC’s program differs
Employing dialectical behavioral therapy (DBT), the premier treatment package for suicidal adolescents, CHOC’s IOP is held four days a week for eight weeks during after-school hours. Programming includes caregivers and a variety of experiential activities. Family sessions are held as needed and optional group programming for graduates is offered.
Phone coaching is also available to allow IOP patients access to their clinicians outside of program hours to gain coaching in moments when they really need it.
By contrast, a traditional DBT program – the most widely researched – is held over a 16-to-32 week period with one weekly individual session and one weekly skills group session that includes caregivers. A 16-to-32 week graduation program and phone coaching, follow.
“This means that the clinical service CHOC provides is delivered in one-quarter to one-eighth of the amount of time as a traditional DBT program, and at a much greater intensity,” Dr. Thordarson says. “So, despite the significantly shorter time period, we are still able to get meaningful outcomes.”
Patients served
Here’s a snapshot of the population served by CHOC’s program during the approximate two-year period:
- The IOP served 105 patients.
- 65 percent of patients identified as female, 27 percent identified as male, and 8 percent identified as gender nonconforming.
- 39 percent of patients were white, 31 percent were biracial, 21 percent were Latino, and 9 percent were Asian.
- 52 percent of patients were referred from a higher level of care, such as an inpatient psychiatric unit or a residential treatment program; 17 percent from the emergency department; 21 percent from outpatient providers or from school; and 10 percent from other sources. This is significant because it means about half of the teens who are admitted to IOP are able to be diverted from an inpatient hospitalization by accessing the IOP-level of care.
- About 80 percent of participants graduated from the program, 11 percent discharged against clinical advice, 7 percent needed a higher level of care, 2 percent needed a lower level of care, and 1 percent required a transfer for specialty care.
Measuring progress
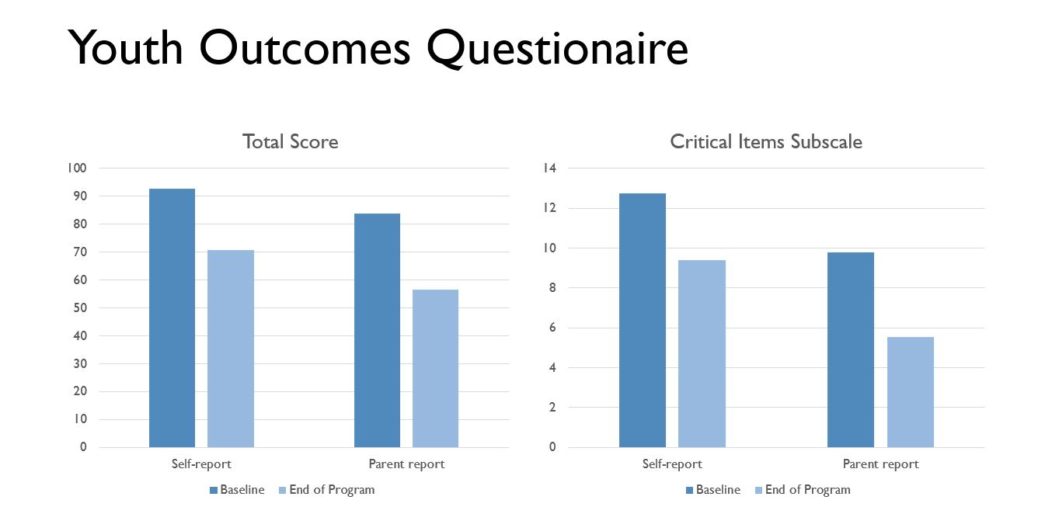
To measure patients’ progress over the course of their time in program, teens and their parents complete the Youth Outcomes Questionnaire 2.0 (YOQ). The YOQ is a broadband measure of emotional and behavioral functioning that includes six subscales: intrapersonal distress, somatic symptoms, interpersonal relationships, social problems, behavioral dysregulation and critical items. Higher scores indicate greater distress.
At the start of the IOP, patients on average self-reported a total distress score of 92.8. At the end of the eight weeks, patients self-reported a mean score of 70.61.
Their parents reported a baseline assessment of their children’s total distress at 83.8 on average and at the program’s conclusion, reported a mean score of 56.39.
Looking more closely at the critical items subscale – which assesses suicide, self-harming behaviors, and other high risk indicators – patients at the beginning of their program reported on average a score of 12.75, followed by a mean score of 9.41 at the conclusion of their program.
Parents reported a baseline critical items subscale score of 9.78 on average, followed by a mean score of 5.53 at the program’s conclusion.
”We were table to analyze these numbers to determine not only whether they were statistically important changes, but also whether they were clinically meaningful,” Dr. Thordarson says. “These changes represent medium-to-large effect sizes. In other words, they demonstrate moderate-to-significant changes in reported distress.”
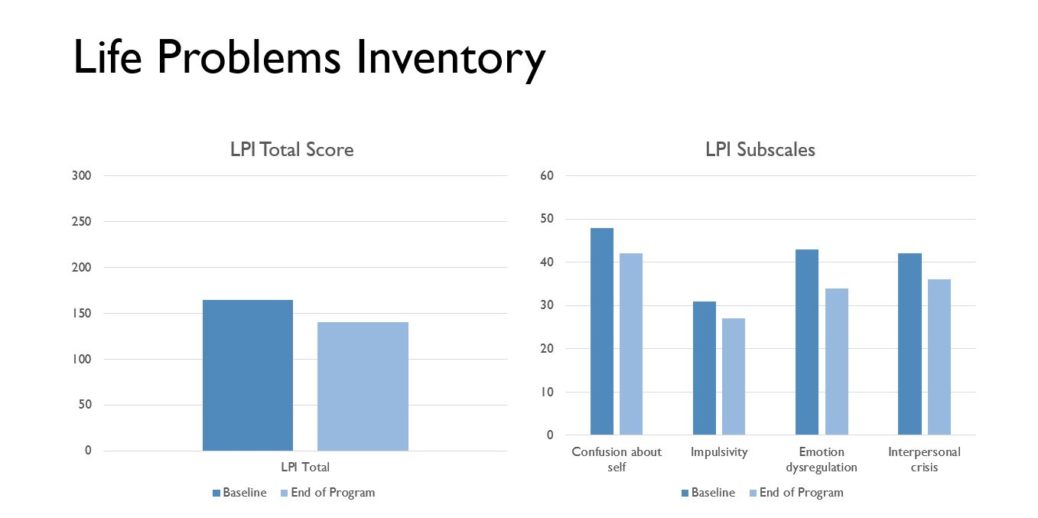
As another means of assessing program progress, patients also completed the Life Problems Inventory (LPI), a measure of the skills deficits that are specifically targeted by DBT. Like the YOQ, higher scores indicate greater distress as well as less employment of adaptive skill use.
At the beginning of the program, patients self-reported a total mean score of 164.26; at the end, 140.
In looking at the LPI’s subscales, each decreased across the board: on average, confusion-about-self scores dropped 5.65 points; impulsivity decreased by 4.19; emotion dysregulation decreased 8.22; and interpersonal crisis dropped 6.2. These changes also represent small-to-large effect sizes.
Next steps
Looking forward, clinicians hope to gather long-term data with several goals in mind: to further assess the effectiveness in continued suicide prevention; determine any difference in outcomes when the IOP was augmented with phone coaching; review data to determine ways to further enhance the program; and continue efforts to build a referral network for ongoing family support after program completion.
“We are so thrilled to offer a very important service to teens and families who are in crisis and need extra support,” Dr. Thordarson says. “The team at CHOC is unparalleled in its enthusiastic dedication to innovation and excellence in the care of children.”
The IOP is a component of CHOC’s landmark pediatric mental health system of care launched in spring 2015 to ensure children, adolescents and young adults with mental illness get the health care services and support they need.
Learn more about CHOC’s intensive outpatient program.
Outpatient providers interested in receiving referrals from the IOP should email [email protected].




