In a collaborative effort from neurology, neurosurgery, emergency medicine, radiology, nursing, and multiple staff across departments, CHOC unveiled a set of updated and improved care guidelines for acute stroke diagnosis and management for pediatrics in February 2022.
Dr. Rachel Pearson, director of brain injury medicine at CHOC’s Neuroscience Institute and co-author of the protocol, explains that after two years of diligent work, the acute stroke guidelines were approved by CHOC’s evidence-based medicine committee and the critical care committee.

Since the protocol’s inception, the team has been collecting data to determine how many ischemic and hemorrhagic strokes have been identified via stroke codes, as well as other abnormal findings, times to assessment and imaging. The team is using the data to inform CHOC’s processes of care, hospital-wide education, and community outreach regarding stroke signs and symptoms in children.
Additionally, CHOC has joined the International Pediatric Stroke Study, an international, multi-site longitudinal observational study of pediatric stroke patients. CHOC’s involvement in this study offers the opportunity to collaborate with publications, and to participate in clinical trials with other national and international sites.
A need for pediatric-focused acute stroke care guidelines
“Just like the care guidelines for traumatic brain injuries, status epilepticus and other disease processes that have a hospital-wide treatment approach (or care pathway), we created the same for acute stroke care,” says Dr. Pearson.
There had been one prior set of guidelines for acute stroke care at CHOC, but it was one page as opposed to the seven that the new one is. The prior guidelines were vague, and our data showed that they weren’t effectively identifying and diagnosing patients who could be candidates for acute intervention.
Now, the updated care guidelines approach patients with potential strokes to identify those that may be eligible for acute intervention. The interventions that are used in adults – like tissue plasminogen activator (tPA), a drug used to break up a blood clot and restore blood flow to the brain, and endovascular thrombectomy (EVT) – haven’t been validated in children with randomized controlled trials but they are considered generally safe based on the data collected. These interventions are being used across various pediatric institutions and have improved outcomes for patients suffering from acute stroke.
Along with the guidelines, the stroke team created four order sets for acute stroke care for use in the emergency departments, inpatient units, tPA and subacute stroke work-up. The team also created a hospital-approved tPA policy to use tPA for pediatric patients, and consent and education for patients in English and Spanish.
The focus of the updated guidelines and order sets is to improve the process of care from the time a patient has a symptom of a stroke at home or at school through their evaluation in the emergency room.
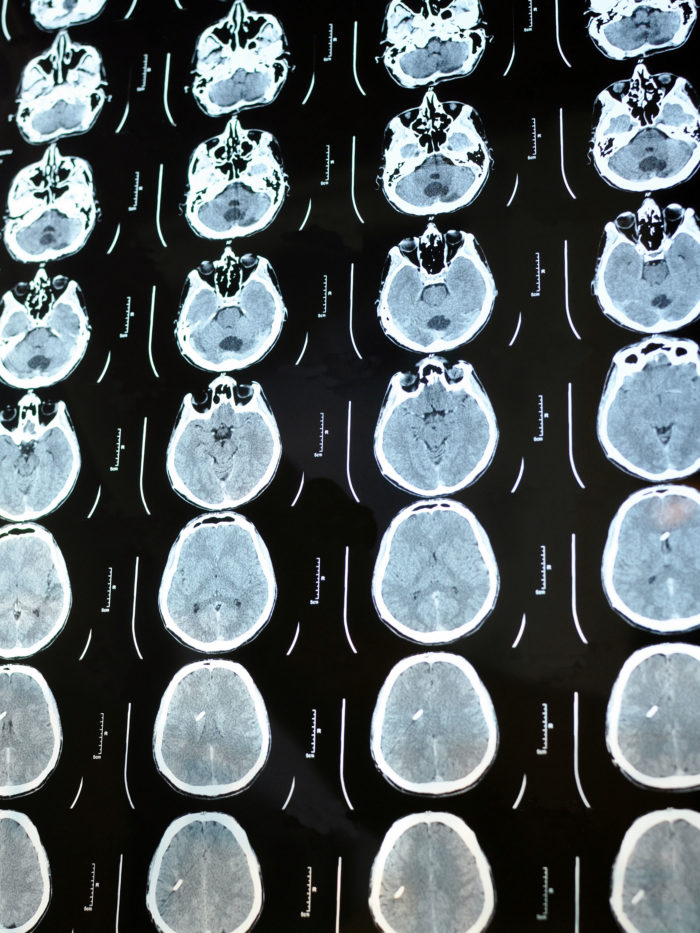
“Making the process of care run more smoothly is essential for improving patient outcomes,” says Dr. Pearson. “With strokes, time is brain. With a large stroke, a patient will lose approximately 2 million brain cells every minute. The faster we can diagnose a stroke in a child, the bigger the difference we can make in terms of neurological outcomes.”
Detecting pediatric strokes can challenging
There are many conditions that mimic pediatric strokes migraine, seizures, and Bell’s palsy. It is vital to have protocols for identifying patients at the highest risk for stroke and getting them diagnosed as quickly as possible. If providers assume that there is always another diagnosis, they’re going to miss the few cases that are actual strokes.
If patients over the age of 2 years present with focal neurological deficits like weakness, sensory change on one side of the body, vision change, speech difficulties, dizziness or trouble walking — that started suddenly and within the last 24 hours — then they’re immediately activated as a stroke code by the provider. They then undergo emergent neuroimaging and, if they’ve had a stroke, a team of doctors determines if they are candidates for any acute intervention.
Since February, CHOC has had a total of 45 stroke code activations. Out of those 45, two patients were diagnosed with ischemic strokes, two with hemorrhagic strokes, and ten with other abnormal findings like brain tumors, aneurysms, encephalitis or autoimmune processes that need to be addressed urgently.
“Compared to retrospective data, these numbers are in line with what CHOC typically sees — five to eight ischemic strokes in children (ages 1-18 years) per year, keeping in mind that not all strokes we see present acutely as a ‘code stroke,’” says Dr. Pearson.
For all stroke codes, certain quality improvement metrics are tracked: how long it takes from the time the patient arrives at the ED to activate the stroke code; the amount of time it takes to secure an MRI; and how long it takes for a neurologist to evaluate the patient; how well the pediatric NIH stroke scales were being used to seek supportive care; and if the patient was being discharged on anti-thrombotic medication. For inpatient stroke codes, the time that it takes for the rapid response team to activate the code is measured as well.
Working toward standardized pediatric-focused stroke guidelines
Since there are no standardized care guidelines or certification for pediatric stroke programs yet, we analyzed the adult-focused guidelines from The American Heart Association (AHA), Joint Commission and others to determine how they could be applied to kids, says Dr. Pearson.
Once we looked through all the metrics from adult-focused stroke guidelines, we brought those to CHOC’s stroke core group— a multidisciplinary group of providers from neurology, neurosurgery, radiology, nursing, hospital administration and the emergency department — and we all decided on a set of similar metrics so we could compare CHOC’s data to national standards.
With most pediatric stroke guidelines being institution-based, CHOC has actively collaborated other institutions that have pediatric stroke expertise – Lucille Packard Children’s Hospital Stanford, St. Louis Children’s Hospital, Children’s National Medical Center, Seattle Children’s, and UCSF Benioff Children’s Hospitals —and have been fortunate to be able to work with them to build our own guidelines and QI database, says Dr. Pearson.
Stroke protocol implementation and results at CHOC
Several layers of education were involved to implement these guidelines at CHOC. First, the guidelines were presented to physicians and advanced practice practitioners at division meetings. Then, the nursing staff completed a mandatory computer module training. In addition, the team has educated the community about CHOC’s stroke care guidelines at Regional Emergency Advisory Committee Meeting and the Orange County Stroke Society.
Every time a stroke code occurs, Dr. Pearson and Stroke Program Supervisor Rowena Roque review the available data about the stroke – how the stroke code was called; what the patient was ultimately diagnosed with; and the amount of time it took to get a diagnosis and treatment — and they enter the information into a feedback form with the metrics and how the team is adhering to the guidelines. Then, that information is shared with the providers on the care team for continued education and feedback to improve the guidelines and find any gaps or barriers to getting patients the appropriate care.

With the comprehensive education on the stroke care guidelines at CHOC, there have been positive results. Activation of the stroke code is happening more expeditiously, and the process for getting timely diagnostic imaging is much smoother than it was in the past.
“These guidelines are a big step in the right direction,” says Dr. Pearson
What’s next in store for CHOC’s stroke program
The cerebrovascular program at CHOC is working to create an outpatient, multidisciplinary neurovascular clinic that will begin accepting patients in January 2023.
The clinic will welcome any cerebrovascular patients with ischemic strokes, bleeds, Moyamoya disease, other arteriopathies, and even perinatal strokes. The clinic will include neurology, neurosurgery, physical medicine and rehabilitation so patients can have a one-stop shop after they’re discharged to see all of their providers in one visit. It will be a significant service for patients to streamline their appointments and will be especially helpful for patients that may have mobility issues as a result of their stroke.
In addition, CHOC’s Stroke team continues to engage with the wider pediatric stroke community in research and will soon be launching a study of a pre-hospital processes-of-care intervention aiming to improve rapid detection of stroke in children with acute neurological symptoms. This is an exciting collaborative effort between CHOC, UCSF and UCLA and has potential to change the landscape of pediatric care on the national level.

CHOC Hospital was named one of the nation’s best children’s hospitals by U.S. News & World Report in its 2025-26 Best Children’s Hospitals rankings and ranked in the neurology/neurosurgery specialty.