Pediatric neurosurgery: Innovating for child-friendly care
Using laser interstitial thermal therapy (LiTT), responsive neurostimulation (RNS) and deep brain stimulation (DBS), pediatric neurosurgeons at Children’s Health of Orange County (CHOC) have been able to improve seizure control and enhance quality of life for patients with epilepsy. The pediatric epilepsy team uses a collaborative approach to help identify patients who are good candidates for surgery which could include resection, ablation using LiTT, or neuromodulation, which includes RNS or DBS.
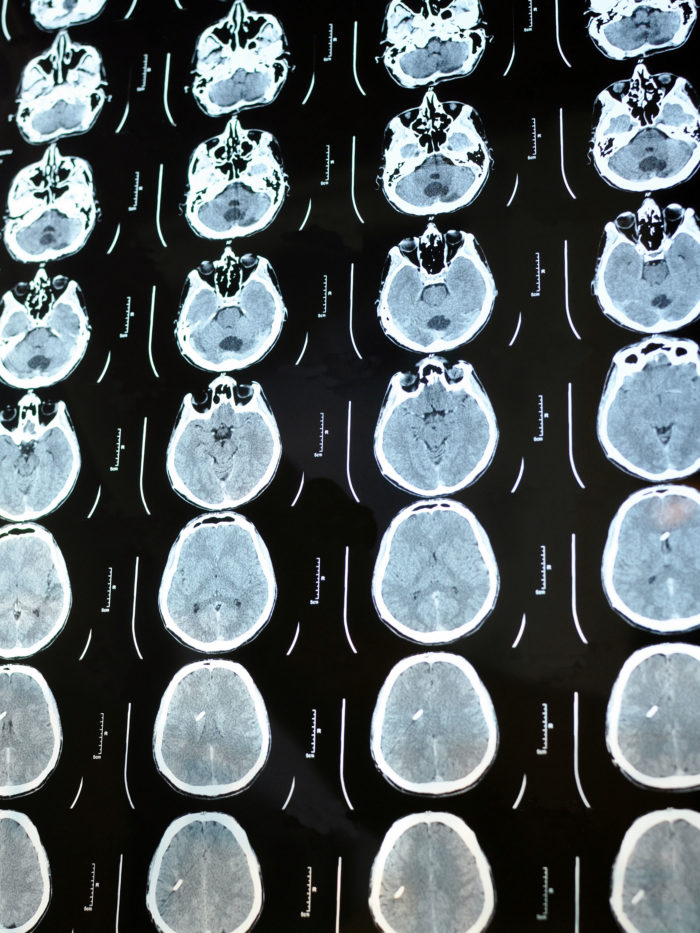
Dr. Joffre Olaya, pediatric neurosurgeon at CHOC, says that careful patient selection helps deliver positive outcomes. When epileptologists identify a patient with intractable epilepsy who has not benefitted from at least two seizure medications, they initiate a detailed workup — continuous video EEG monitoring, a brain MRI, a PET scan and occasionally a single photon emission CT (SPECT) scan or magnetoencephalogram (MEG). Combining or “co-registering” these studies helps localize where seizures are originating in the brain. Patients also undergo neuropsychiatric evaluation to help map brain function. Neurosurgeons and epileptologists partner closely in the presurgical workup and treatment plan.

Laser ablation
For patients with small focal lesions in the brain, LiTT, or laser ablation, is less invasive than open craniotomies and resections. Pediatric neurosurgeons make a small incision and a burr hole, then use robotic stereotactic assistance (ROSA) to help plan the entry point and the target for probe placement.
“It’s nice because it’s minimally invasive — a smaller incision, typically shorter hospitalization, less pain and less blood loss,” Dr. Olaya says. “There are definitely a lot of benefits to laser ablation in the appropriate candidate.”
Sometimes laser ablation is preceded by a trial using temporary depth electrodes placed using ROSA. After the electrodes are placed, the patient is admitted and seizure activity is monitored. If seizures originate from a focal area, the temporary depth electrodes are removed, and the patient returns for laser ablation after recovering from the initial trial. While laser ablation is not appropriate for every seizure patient, it can be very beneficial for those with a focal epileptogenic zone.
Recently, Dr. Olaya has been performing corpus callosotomy using laser ablation for drop seizures. Classically, this procedure was performed as an open craniotomy to disconnect the corpus callosum between the hemispheres of the brain.
“Now, using three or four trajectories with the laser probe, we can accomplish the same endpoint,” Dr. Olaya says. “By making three or four small incisions, placing probes and disconnecting the corpus callosum, we can have a dramatic effect on seizure control. This can shorten hospitalization and recovery times.”
Neuromodulation: Responsive neurostimulation (RNS)
Responsive neurostimulation (RNS) is FDA-approved for patients ages 18 and older, but CHOC offers this treatment to pediatric patients ages 12 to 17 through a multicenter clinical trial. RNS involves placing strip electrodes over the surface of the brain or implanting depth electrodes to target deeper brain structures. Powered by a small generator implanted in the skull, the device records electrical activity and sends electrical stimulation to shorten or stop a seizure when one occurs.
RNS can be beneficial for pediatric patients with multifocal epilepsy or those who have a focus for which surgical resection could potentially cause neurologic deficits, especially those near the language centers or motor cortex. RNS can help clinicians surgically treat seizures without causing neurologic injury.
Neuromodulation: Deep brain stimulation (DBS)
Deep brain stimulation (DBS) can be used for movement disorders, but it can also be used to treat intractable pediatric epilepsy. DBS placement requires two stepwise surgeries: one for lead placement and the other for generator placement. During the first surgery, ROSA is used to precisely place electrodes down to the target, typically the anterior thalamus. Electrodes are secured and the end of the wires are tunneled posteriorly to the back of the head. After a week or two, a second surgery is performed to implant an extension wire and tunnel it down to a generator placed in the chest.
Improved seizure control can help with childhood development, including language skills and socialization; these less invasive surgical options may be the key to reducing seizures and improving quality of life in pediatric patients with epilepsy.
“These procedures [laser ablation and neuromodulation] make a huge difference in our patients’ lives,” Dr. Olaya says. “I just saw a patient recently for whom we performed a laser ablation corpus callosotomy. She had been having frequent drop seizures, hitting her head all the time. Her parents had to be at her side constantly. After we performed the procedure about three months ago, she has been like a different person. Her mother took her to a birthday party for the first time. I have endless stories like this where getting their seizures under control made a huge impact on the patient’s and family’s life.”
Learn more about CHOC’s minimally invasive neurosurgery program

CHOC Hospital was named one of the nation’s best children’s hospitals by U.S. News & World Report in its 2025-26 Best Children’s Hospitals rankings and ranked in the neurology/neurosurgery specialty.