The Adolescent and Young Adult (AYA) Treatment Program at the Hyundai Cancer Institute at CHOC has invested in new modalities for psychosocial patient support during the ongoing COVID-19 pandemic with surprising success.
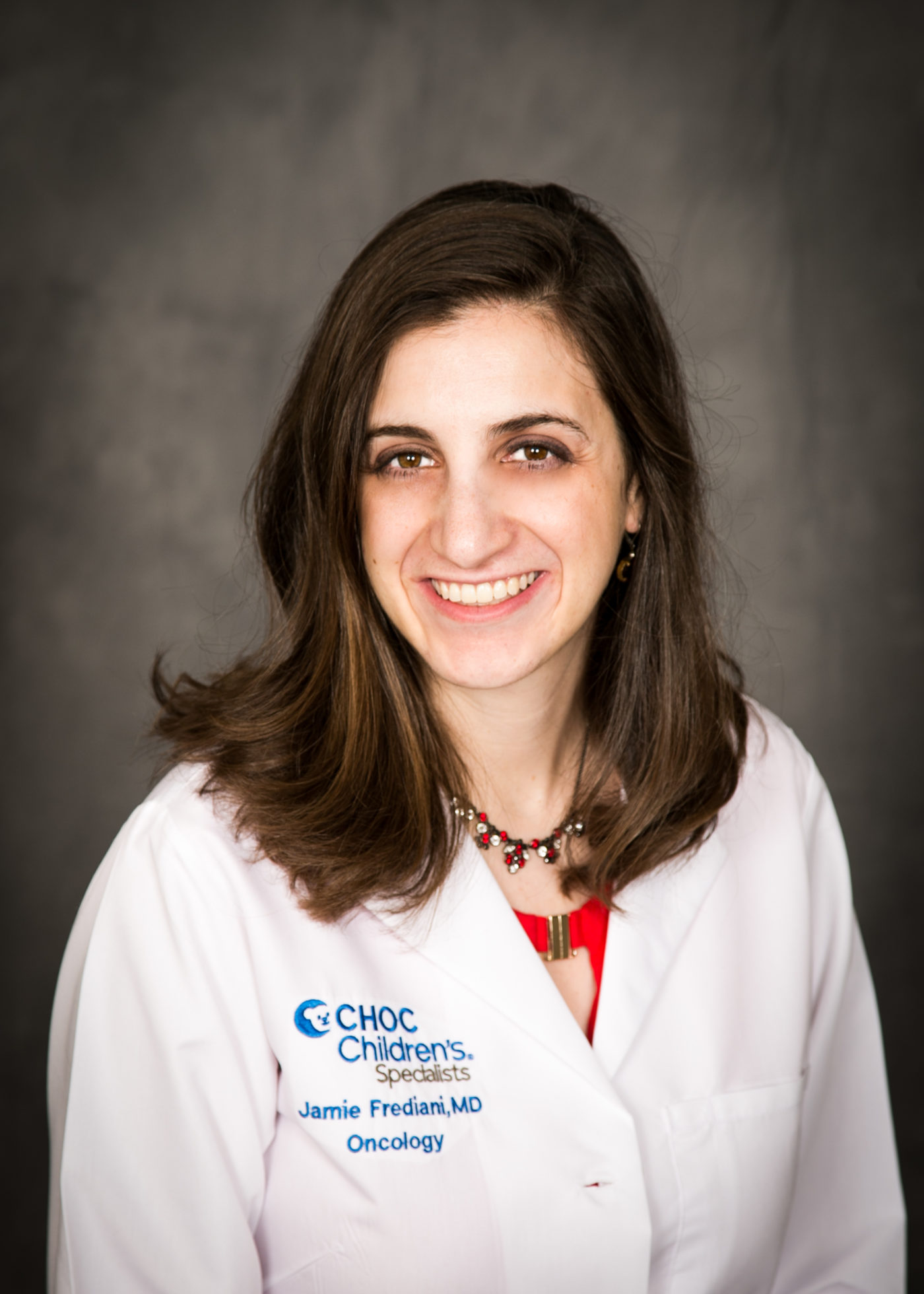
“In general, adolescents and young adults need significantly more psychosocial support and guidance than a younger patient does,” says Dr. Jamie Frediani, board-certified pediatric oncologist at CHOC. “For the past 10 years at CHOC, we have focused on trying to meet their psychosocial needs as well as provide them with unique treatment and clinical trial opportunities in order to give them a better overall survival and better mental health outcomes. When COVID-19 happened, we went from having a large amount of support for these patients to having very little support for them — all while they were having heightened feelings of anxiety and depression due to pandemic-imposed isolation.”
Chats, classes and increased connectivity
Prior to March 2020, CHOC hosted activities for AYA patients at least twice a month on average. The pandemic ended in-person group events, and limited one-on-one in-room activities for hospitalized patients.
“We said, ‘Let’s move [our AYA programming] virtual,’ since everything else in the world was moving virtual at the time,” Dr. Frediani says.
CHOC had not used Zoom for psychosocial support services before but began to host a weekly coffee chat on Friday mornings for AYA patients. Turnout kept ticking upward, so Dr. Frediani’s team organized a series of game nights, education sessions and holiday events. This evolved into a series of virtual cooking, art and crafts classes, where supplies could be picked up in advance.
“We had a lot of kids who got more involved, because it was easier for a kid who was in active treatment or in the hospital to join a Zoom call where they could leave the camera off than it was for them to put on real clothes and drive all the way down to the hospital in person,” Dr. Frediani says. “We also found that families who live farther away or who have transportation issues became active participants when they hadn’t been before. For us, the programming during the pandemic wasn’t just a lesson in creativity. It really paid dividends, because we got some kids involved and engaged in a way that we hadn’t seen before.”
Starting a band
Even before 2020, providers and interested AYA patients had planned to start a band as part of CHOC’s music therapy program. The pandemic meant the band went online, too. Even virtually, the band showed promising results.
“The AYA Oncology Band presented a unique opportunity for our patients to develop skill mastery, foster relationships, minimize social isolation and process their emotions in a positive therapeutic space,” Dr. Frediani says.
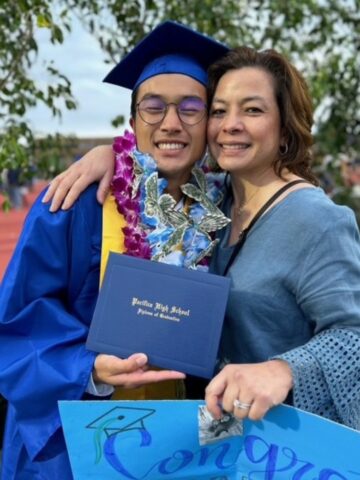
Meeting bimonthly from March 2020 to August 2021, 23 patients played instruments, sang, created a logo, planned performances and learned how to record them.
“The idea was to learn coping skills through music, while also interacting with a supportive community in a very neutral setting,” Dr. Frediani says. “We hoped our patients would be able to feel some of that sense of achievement that cancer really strips away. [The band] exceeded all of our expectations.”
Many participants reported dramatic subjective changes, as feelings of efficacy replaced helplessness and joy replaced loneliness.
“I felt isolated and alone before joining the AYA band, but after having the opportunity to create music with a group of people, I felt the joy of being a part of a group again and found a sense of belonging,” one patient explained.
“The fact that I was able to learn how to play an instrument that I had never even touched before was really empowering,” another patient said. “Realizing my capability of doing something on my own, especially at times when I was feeling weak and helpless, really ignited the thought, ‘I got this! I can do this!’ and encouraged me to persevere through my treatment.”
Dr. Frediani has witnessed many similar transformations.
“I think that that’s a lot of what we see with these programs,” she says. “It’s not just whether or not the cancer treatment works — it’s promoting feelings of togetherness, self-mastery and accomplishment while restoring what cancer takes away.”
Future outcomes and research
Pediatric and adult cancer patients have made great gains in survival rates in the past 20 years, but AYA outcomes have lagged. Some of these numbers are due to different types of tumors and other multifactorial reasons, but access to mental health services, such as psychosocial support, also seems to affect outcomes for some AYA patients.
“Psychosocial programming makes a dramatic impact on the lives of our cancer patients,” Dr. Frediani says. “They need to know that they are not in this alone. They need to know that other kids have done this before them.”
While the anecdotal evidence suggests virtual programming has played an important part in improved emotional outcomes during the past two years, Dr. Frediani plans to further research CHOC’s psychosocial programs to better quantify metrics in relation to outcomes, so that other programs can adopt them. Dr. Frediani will present her observations about CHOC AYA virtual programming at the 2021 Global Adolescent and Young Adult Cancer Congress in December.
“Every AYA in the nation should have access to this type of support,” Dr. Frediani says. “I believe that in sharing this information, we do the best service to the greatest number of patients.”
Learn more about the Adolescent and Young Adult Treatment Program at CHOC.

CHOC Hospital was named one of the nation’s best children’s hospitals by U.S. News & World Report in its 2025-26 Best Children’s Hospitals rankings and ranked in the cancer specialty.