CHOC utilizes innovative treatment plans for scoliosis in pediatrics
As scoliosis surgery has evolved since the mid-20th century, one fact has become clear: The success of the operation hinges on restoring sagittal alignment of patients’ spines. Advances in biplanar imaging have revealed that, in patients with scoliosis, not only does curvature occur in the body’s coronal plane, but the spine also loses much of its natural kyphotic curvature, according to Dr. Afshin Aminian, board-certified orthopaedic surgeon and medical director of the CHOC Orthopaedic Institute. Both require correcting.

“When we seek to correct the scoliosis deformity, one of our main goals is not just to get it straight in the coronal plane but also to restore the sagittal alignment,” Dr. Aminian says. “We have to restore the thoracic kyphosis. If we don’t, then we don’t get the compensatory changes in the unfused segments in the cervical and lumbar spine. Hence, the patient looks good and has a great frontal X-ray, but if you don’t have that sagittal alignment restored, you don’t get the compensatory changes in the unfused segments. As a result, a child potentially ends up with early degenerative changes and problems in the unfused segments as they get older.”
The CHOC Orthopaedic Institute was one of the first centers in the U.S. to focus on planning for and restoring sagittal alignment using personalized, pre-shaped implants, beginning in 2016. Two years later, the institute took scoliosis surgery innovation a step further by using patient-specific rods and artificial intelligence (AI)-driven machine learning and predictive modeling to optimize spine alignment.
Personalized and predictive spinal rods for scoliosis surgery
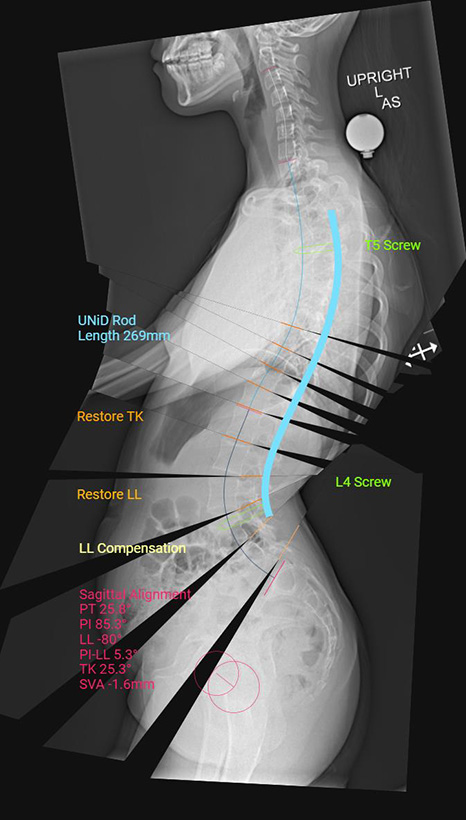
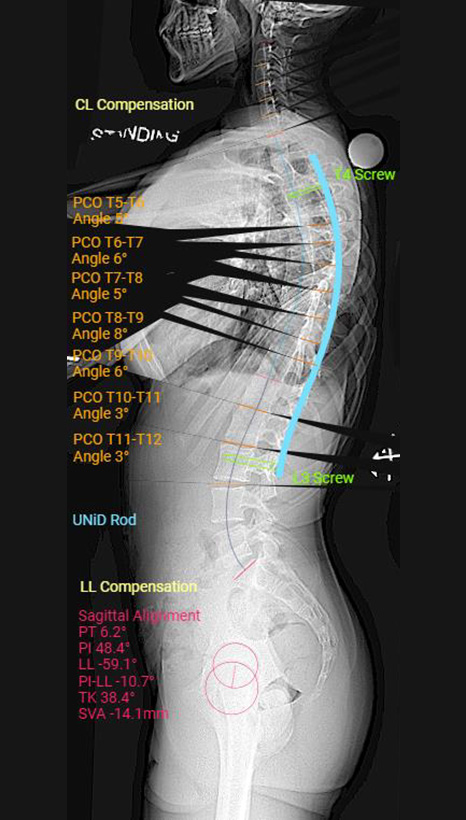
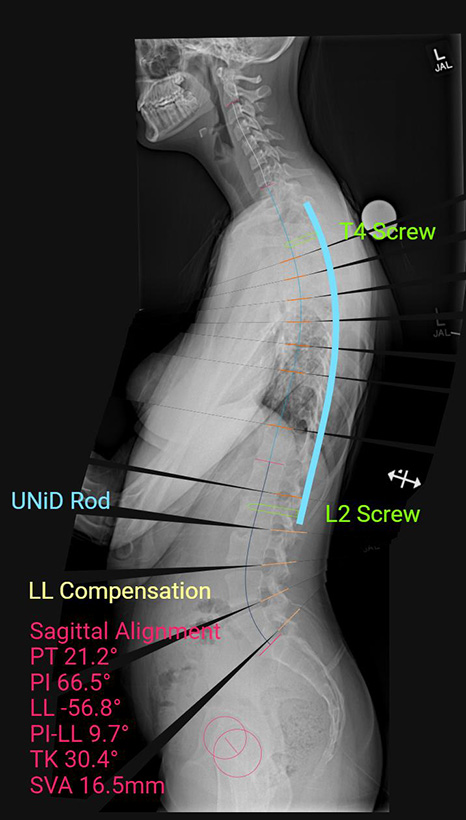
The UNiD™ Adaptive Spine Intelligence AI platform by Medtronic, which features a database of more than 10,000 spine surgeries according to Dr. Aminian, allows him to use patients’ X-rays to plan operations and design customized spinal rods.
“We take the lateral radiograph, and we know the segments we’re going to fuse based on our frontal X-ray and other bending parameters,” Dr. Aminian says. “Then, we turn to the sagittal alignment and say, ‘OK, we’re going to fuse the spine probably from T4 to L1,’ but that thoracic spine is usually lordotic. Usually, patients are hypokyphotic in those segments, and we want to restore the thoracic kyphosis to a normal alignment of, let’s say, 30 degrees.”
This is where UNiD’s predictive modeling comes in. Running the surgical plan through the program allows Dr. Aminian to see what the spine would look like if he were to perform a particular type of surgery.
“I can then go back and say, ‘This doesn’t look so good. I’m going to do 35 degrees instead because now this looks a lot better — better alignment in the relationship to the lumbar spine, the pelvis and the global alignment in the sagittal plane,’” he says. “I get to dial in the appropriate thoracic kyphosis to get in the perfect sagittal alignment.”

Using personalized rods that arrive pre-bent to the shape Dr. Aminian specified in the computer eliminates the need to measure and cut the rods intraoperatively, as surgeons previously had to do. Intraoperative bending left notches in the rod, reducing its mechanical soundness, Dr. Aminian says.
“I have data on each rod,” he says. “I’m not just blindly bending the rod. I know its exact specifications as far as the shape, contour, alignment and all the different angles, so then I get to evaluate the postoperative alignment.”
That, crucially, allows the surgeon to constantly improve the surgical technique.
Promising results for patients with idiopathic scoliosis
Recently, the European Spine Journal published a study presenting the results of Dr. Aminian’s first 48 cases using custom implants and predictive modeling in patients with adolescent idiopathic scoliosis. The study showed improvement in a variety of patient-reported outcomes, including pain, function, mental health and self-esteem. Just as important were the study’s findings related to restoration of sagittal alignment.
“Prior to our study, many studies showed that trying to restore the sagittal alignment and proper kyphosis resulted in deformity and shape changes,” Dr. Aminian says. “In our study, however, with the use of patient-specific custom rods, we showed that we were able to restore the planned kyphosis with minimal change in the shape of the rod.”
Innovations in scoliosis treatments without surgery
Surgery isn’t necessary or appropriate for every patient with scoliosis, which is why CHOC is heavily invested in researching nonoperative management and making the latest advancements available. These include the Schroth Method, a type of physical therapy that uses low-impact exercises and breathing techniques to strengthen spine-adjacent muscles and correct posture.
Machine learning and AI don’t just inform scoliosis surgery decisions at CHOC. They also contribute to better braces.
“We’re incorporating systems to use data collection, machine learning and AI to improve bracing design to make it more user-friendly and get optimal correction. Our goal is to prevent children from progressing to the stage where they need surgery,” Dr. Aminian says. “Some newer AI methods can also aid in the early detection of scoliosis and improve early bracing and nonoperative management.”
In another effort to help orthotists produce more effective braces, CHOC researchers are studying surface sensors placed on the spine to see if they can create a real-time, 3D model of how the spine reacts to pressure in different areas. This could help orthotists fine-tune the shape of braces to achieve the best possible correction.
Learn more about CHOC’s Orthopedic and Sports Medicine Services
Our team of board-certified specialists and orthopaedics-trained staff provide a full spectrum of care for disorders of the bones, joints, ligaments, tendons and muscles.




