From helping clinicians diagnose undiagnosed mental health conditions to catching hard-to-detect lesions in colonoscopy patients, powerful computer algorithms continue to provide potentially groundbreaking opportunities for researchers with their ability to harness massive amounts of data.
This was a key takeaway of Research Day 2022, CHOC’s annual free webinar that this year focused on how computing and data science holds promising solutions to challenges in pediatric medicine.
“We have many children that we know how to care for, but many more we are learning about how to care for and we always need to be improving – it’s our mission to go beyond,” CHOC Chief Scientific Officer Dr. Terence Sanger said in opening remarks at the all-day event Nov. 16 that brought together researchers, clinicians, staff, computer and data scientists and students to share their knowledge, research, and experience.

Data science is an intrinsically interdisciplinary field with the potential for wide-reaching, scalable impact, and the CHOC Research Institute has been on the cutting edge of increasing access to data science.
Assisting clinicians with artificial intelligence
Grand rounds speaker Dr. Aldo Faisal, a professor of artificial intelligence and neuroscience at Imperial College London who has collaborated with Dr. Sanger, discussed how machine learning is helping clinicians make more informed decisions.
“This is one of the biggest shifts in how we develop solutions since the invention of fire,” Dr. Faisal said of machine learning, a branch of artificial intelligence (AI) and computer science that focuses on the use of data and algorithms to imitate the way that humans learn, gradually improving the accuracy of the algorithms.
“It’s not the engineer coming up with something — it’s the data telling us,” Dr. Faisal said. “You learn the solution from the data.”
Dr. Faisal discussed his AI research involving artificial or bionic pancreases, systems that monitors blood glucose (sugar) levels automatically and provide insulin to people with Type 1 diabetes.
In a study using animal models, the system learned algorithms that controlled the proper amount of insulin needed to be injected to keep glucose levels stable.
“This is an example of reinforcement learning in medicine,” Dr. Faisal explained. “AI in healthcare is not about replacing doctors or nurses, but about helping to address the unmet clinical demand that has been growing and will further grow, therefore freeing up the time of clinicians to focus on other complex problems.”
Another of Dr. Faisal’s studies involves using AI to assist clinicians in providing as little anesthesia as necessary during surgeries, while another research project involves helping to diagnose patients in intensive care units with sepsis.
“These systems recommend treatment (strategies) to doctors and they can choose whether to follow them or not,” Dr. Faisal said. “These systems are learning from historical operational data, not patient/doctor interactions.”
Strength in numbers, meaningful data helps find biomarkers for infantile spasms
“Computer Vision in Pediatric Medicine and Science” panel moderator Dr. Peter Chang, co-director of the Center for Artificial Intelligence in Diagnostic Medicine at the UC Irvine School of Medicine, said CHOC is developing a core of data scientists to help facilitate this type of work.
Computer vision refers to the ability of computers to derive meaningful information from digital images.
“Now, the models are driven by data – you don’t need a lot of input from humans,” Dr. Chang said.
CHOC’s Dr. Daniel Shrey, a neurologist and epilepsy specialist, discussed a multi-center, national study he’s leading to find predictive biomarkers for infantile spasms.
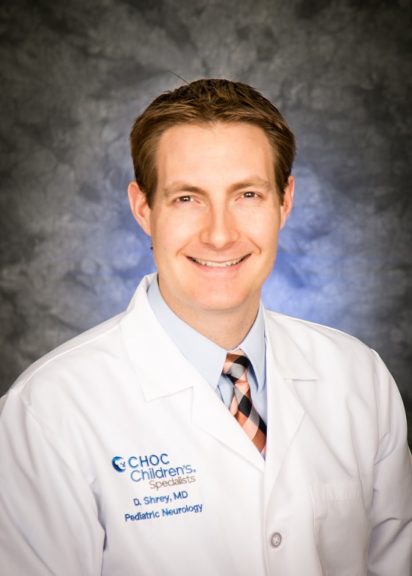
“If one were to do this in a silo,” Dr. Shrey noted, “it would take one person’s entire career. The multi-center approach helps immensely.”
Because there are more than 300 known causes of infantile spasms, clinicians need to look at a lot of patients to extract meaningful data, Dr. Shrey said in his presentation, “Strength in Numbers: Discovering Biomarkers for Rare Epilepsies.”
He and his collaborators are creating a master database of information from more than 600 pediatric patients at CHOC and 20 other hospitals to detect predictive biomarkers for infantile spasms so the condition can be treated as early as possible.
A more complete picture, cardiac MRI imaging
Cardiologist Dr. Pierangelo Renella, director of the Cardiac MRI Program at CHOC, discussed “Computer Vision in Pediatric Cardiac Magnetic Resonance Imaging.”
Dr. Renella noted how, in 1984, the debut of cardiac magnetic resonance imaging proved to be a huge boon to the field because the new technology allowed doctors to view the intricacies of the heart in in a more comprehensive manner.

But the process still is very time consuming and relatively expensive and resource intensive, especially when studying congenital heart disease, Dr. Renella said.
Computer vision and AI algorithms applied to cardiac imaging may be helpful in detecting congenital heart disease types that are rare, have heterogenous anatomy, have various surgical strategies available and have a paucity of outcome data, he noted.
“In the future of fast and automated processing, with minimal loss of quality, we will be able to decrease technologist and physician ‘busy work’ time and potentially produce more reproducible and accurate results,” Dr. Renella said.
‘Some exciting things’ using AI in gastroenterology
Since 2016, CHOC Gastroenterologist Dr. Kenneth Grant and his team has been collecting data on every outpatient with inflammatory bowel disease (IBD) as part of a quality-improvement program called ImproveCareNow.

“We have some exciting things going on in AI and the GI world,” Dr. Grant said.
AI models are helping doctors identify hard-to-see lesions during colonoscopies and thus aid in diagnoses, Dr. Grant said.
Similar work is being doing with esophageal cancer patients, he added.
Crohn’s disease and ulcerative colitis are classic types of IBD disease, but there are many different subtypes of these ailments, he said.
Dr. Grant said AI models are being used to predict steroid-free remission in IBD patients to facilitate treatment decisions, thus minimizing disease morbidity and promoting prompt, long-lasting remission.
AI modeling is also being tested to determine if more specificity can be brought to both diagnosis and treatment, Dr. Grant said.
Digital imaging of pathology tissue slides, as a standard for CHOC, will offer clinical and research opportunities, he added.
Early-life adversity in children
Pediatric neurologist Dr. Tallie Baram, a Bren distinguished professor and director of the Conte Center at UC Irvine, discussed how computational/epigenetic research can help pediatricians predict for a given child if he or she is at risk of experience adverse childhood events (ACEs), which are associated with poor developmental outcomes.
The goal, Dr. Baram said, is to identify and screen for an actionable type of early-life adversity and verify its influence on neurodevelopmental outcome and design interventions to mitigate it.
CHOC, in partnership with UCI and Chapman University, recently was awarded a $2.3-million grant to study how toxic stress and unpredictability in the early environment affect neurodevelopment.
So far, 13 CHOC primary care clinics throughout Orange County have completed more than 15,000 screenings of children and entered the results into a database. Results of the study are expected by the end of 2024.
In another aspect of the study, cheek swabs from 70 children have been obtained for genomic analysis.
The youth mental health crisis
In the final panel discussion of Research Day 2022, “Natural Language Processing/Understanding,” CHOC pediatric psychologist Dr. Adrianne Alpern noted that 1 out of 5 children is living with a mental health condition, with the most prevalent being anxiety, ADHD, and depression.
In 2019, almost one out of five high school students seriously considered suicide and LGBTQIA+ youth who face stigma, discrimination and rejection are at an increased risk for adverse mental health outcomes, Dr. Alpern said.
She said 42 percent of LGBTQIA+ youth seriously considered suicide in the last year.
“Because we have teams of clinicians and researchers that can do studies grounded in the real world,” Dr. Alpern said, “we are best equipped to collect data.”
Natural language processing (NPL) is useful in the field of mental health because the technology can capture undiagnosed, under-reported events – such as by identifying opioid-related incidents from unstructured text in electronic healthcare records (EHRs) – and social determinants such as poor housing, noted panelist David Talby, PhD, chief technology officer at John Snow Labs, a healthcare-focused AI company.
Grateful clinical trial participants at CHOC
Patrick and Brianna LeMaster spoke at Research Day 2022 about enrolling their son, Christian, now 15 months old, at CHOC in a multi-center clinical trial to test a drug, lacosamide, for infantile spasms in newborns. The drug has received Food and Drug Administration approval for older pediatric patients.
The LeMasters said they chose to be part of the clinical trial to potentially help other kids with the same condition.
Brent Dethlefs, executive director of the CHOC Research Institute, noted that CHOC is committed to looking at questions that arise from the bedside and bringing solutions back to the bedside.
“We never forget at CHOC that our patients and families are front and center with everything to do, and that is certainly true of research,” Brent said.
Learn about pediatric research and clinical trials at CHOC




