The two medical providers ran into each other in the physician dining lounge at CHOC’s hospital campus in Orange, CA.
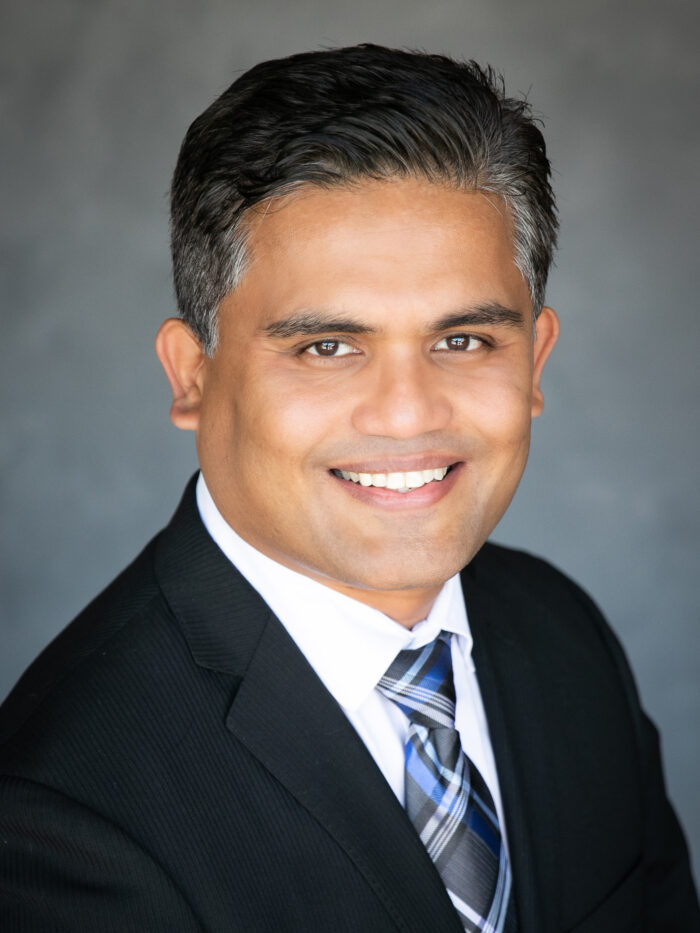
Neurologist Dr. Sharief Taraman, co-director of the CHOC multidisciplinary concussion clinic, took a seat across from gastroenterologist Dr. Ashish Chogle, director of the Functional Abdominal Pain Program at CHOC.

Their discussion turned to a device Dr. Chogle has been using since 2018 to treat patients with irritable bowel syndrome and other functional gastrointestinal disorders including chronic nausea.
Called IB-Stim, it attaches to the ear and electrically stimulates the vagal nerve, the most important nerve of the autonomic nervous system, which regulates the body’s automatic functions involving the heart, lungs, digestive tract, etc.
CHOC was the first pediatric hospital to use the IB-Stim device on patients (outside of a research study) in the U.S., and in many patients, it has eased symptoms of functional gastrointestinal disorders.
Over a casual lunch with Dr. Chogle, Dr. Taraman wondered: Would the device work on patients suffering from Post-Concussion Syndrome (PCS) for their chronic nausea?
“It’s possible,” Dr. Chogle told him. “Let’s try it.”
Chat leads to clinical trial for PCS patients
Dr. Chogle started seeing the PCS patients with chronic nausea in his clinic and he observed that in addition to nausea getting better with IB-Stim treatment, other symptoms of PCS started showing improvement as well.
He recalls the “amazing” effects on the first patient, who couldn’t stand in an elevator without falling to the ground.
After wearing the IB-Stim device, the boy and his parents came into Dr. Chogle’s clinic. Mom and dad were crying.
“I was scared, wondering what happened,” Dr. Chogle recalls. “Then they told me this was the first time in several years that their son hadn’t fallen while riding up in an elevator. He no longer had any balance issues.”
This and similar experiences from Dr. Chogle’s other PCS patients led him to design a clinical trial to confirm his observations.
100 patients to be enrolled
About 15 percent of kids and adults diagnosed with a concussion will develop PCS.
While the underlying cause of PCS remains unclear, dysfunction of the autonomic nervous system is believed to play a critical role. Animal models have found that treating autonomic dysfunction with vagal nerve stimulation improved the speed and extent of recovery after simulated mild traumatic brain injury.
Dr. Taraman’s talk with Dr. Chogle led to a clinical trial now underway, with about 30 patients enrolled out of a planned 100.
Stalled by the COVID-19 pandemic, this investigator-initiated research could lead to breakthrough treatment of PCS, whose symptoms include headache, dizziness, balance issues, fatigue, and problems with concentration and memory that linger three months or longer after a mild head injury.
‘Great potential’ for use of IB-Stim device
Dr. Taraman and Dr. Chogle are fond of coming up with ways to use existing or emerging devices and technology to improve outcomes for their patients (here’s an example and here’s another).
The CHOC Institutional Review Board (IRB) allowed the use of IB-Stim, which had been approved by the Food and Drug Administration for GI issues, for the PCS clinical trial.
The device has wires with tiny needles at the end and is placed on the outer ear. It is worn five days a week for four weeks.
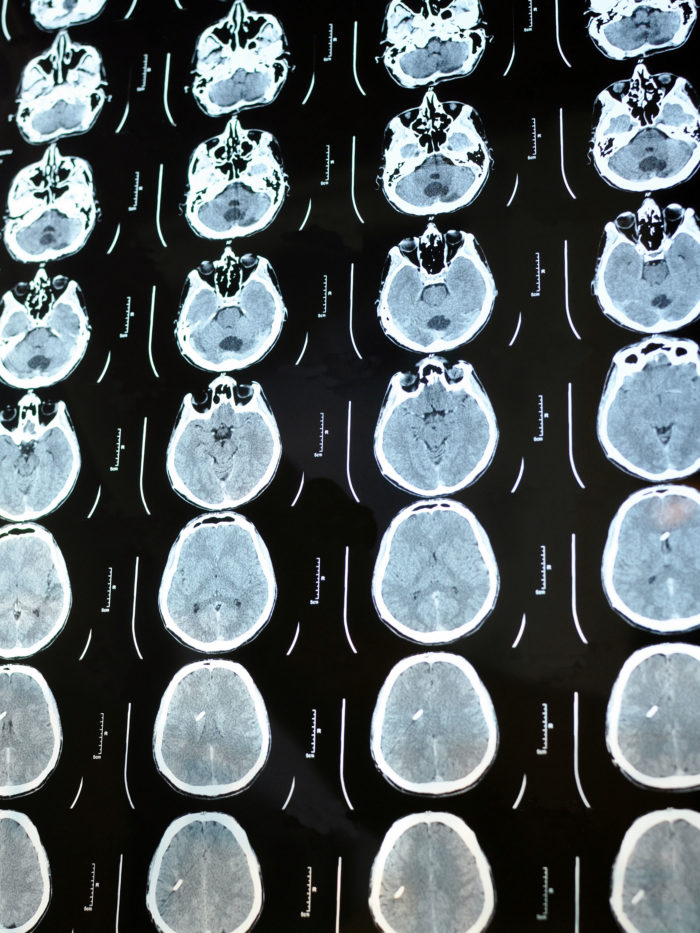
Study procedures in the clinical trial include neurological testing (a balance test and computerized neurological standard testing), cardiac testing (heart rate, blood pressure, electrocardiogram for heart rate variability), eye test (pupillometry), and parent/child questionnaires.
“It looks like it has great potential for PCS,” says Dr. Taraman. “Some symptoms of irritable bowel syndrome overlap with those of concussion syndromes. And the beauty of this medical device is that it can treat a very specific problem without exposing the body to everything that comes with a medication. Medications are not very specific and go everywhere, and you have to think about side effects – that’s a real advantage with this device.”
At first, skepticism of IB-Stim for abdominal pain
Dr. Chogle first heard about the IB-Stim in 2017, when it was being researched at Children’s Wisconsin hospital in Milwaukee for treatment of irritable bowel syndrome. He reached out to the device manufacturer.
“I was a bit skeptical at first,” Dr. Chogle says, “but I’m always looking for newer ways to treat my patients. There are always some patients who don’t get better with conventional treatment.”
Dr. Chogle tested the device on nine of his patients and six got significantly better, he says. He then started using the IB Stim device to treat several of the patients he saw in his Functional Abdominal Pain clinic (one of the only such multidisciplinary clinics for children on the West Coast). Dr. Chogle says, “The IB-Stim became one more tool in my kit to treat my patients.”
High praise from a CHOC nurse with PCS
A CHOC nurse who suffered from PCS and a teenage athlete with a history of concussions and abdominal migraines praised the IB-Stim.
“It’s one of the best decisions I made in my life,” says palliative care nurse Tayler Key, RN, BSN, who suffered from debilitating headaches and other issues after an autistic patient slugged her between the eyes during a blood draw.
Ava “Rosie” Cline, 17, a star volleyball player at Foothill High School in Tustin as well as on an L.A.-based national volleyball team, finally is feeling more herself after several IB-Stim treatments following a harrowing medical journey of many ANS-related symptoms associated with PCS, says her mother, Traci.
“Our doctors at CHOC, there’s none better, honestly,” Traci says. “They’ve gone above and beyond with a powerful drive to heal our daughter from these debilitating PCS symptoms.”
An unfortunate event leads to concussion
One day in early May 2019, Dr. Chogle ran into Tayler while seeing his patients.
Word had gotten around about Tayler’s concussion, suffered in December 2018 at the hands of a combative and uncommunicative teen.
After the teen nearly cold-cocked Tayler between the eyes – because of the teen’s condition, Tayler feels no blame or ill will because of what happened – the nurse saw stars. Despite having a black eye and bruise along the bridge of her swollen nose, Tayler was able to finish the blood draw with the help of security personnel.
Then came the tears.

And the excruciating headaches. The frequent nausea. And the inability to tolerate light or computer or phone screens.
Weeks turned into months.
An irritable and downcast Tayler was far from her usual bubbly self.
Back at work three months after getting hit, Tayler was able to make it through her shifts. But it was tough, despite being assigned to a dimly lit environment.
After hearing her story, Dr. Chogle asked Tayler if she wanted to try out the IB-stim.
“Honestly,” she told him, “at this point, if you tell me to get on my head and do that for an hour a day, I would do it.”
She immediately said yes.
“He was so enormously kind and generous,” Tayler says of Dr. Chogle, who would attach and detach the device on her work breaks, at the nursing station, or in his office.
Dramatic turnaround from anaphylaxis
Rosie’s abdominal migraines began at age 5 but she wasn’t diagnosed with them until she was 11, Traci says.
Rosie also suffered volleyball-related concussions in April 2017 and March 2018, the last of which kept her out of school and volleyball for six months.
Although released from typical concussion protocol, in April 2019 she started experiencing many of the ANS dysfunction symptoms and unexplained, life-threatening anaphylaxis, fainting episodes, and severe gastrointestinal dysfunction.

Anaphylaxis causes the immune system to release a flood of chemicals known as histamine that can cause a person to go into shock. Blood pressure drops suddenly, and the airways narrow, blocking breathing. With the many PCS symptoms, Rosie found herself constantly at doctors, in the ICU and unable to play volleyball or attend school consistently.
In 2021, she stayed twice in CHOC’s pediatric intensive care unit (PICU) and had multiple trips to the ER and hospital stays.
Today, she’s resumed her normal activities including competitive volleyball – thanks to the IB-Stim, which she has used five times since July 2021. Her PCS symptoms have all but disappeared and her energy and focus have improved as well.
“She’s doing amazing now,” says Traci, adding that Rosie’s abdominal migraines are much fewer and far between and her daily upset stomach no longer is an issue. “She can’t remember feeling as healthy as she feels right now and her doctors and IB-Stim deserve most of the credit.”
Laughing again
Rosie and her family still have some PTSD and fears because of the intensity of her prolonged health scares, Traci says, but the 5-foot-9 incoming senior feels great these days and continues to thrive in school, volleyball and teenage living while also focusing on her future college life.


Rosie and her mother praise her team at CHOC, which also includes hematologist Dr. Diane Nugent and Rosie’s pediatrician, Dr. Chris Koutures.
Tayler, meanwhile, says it’s hard to imagine where she’d be today if she didn’t use the IB-Stim device.
“The headaches were so debilitating,” she says.
Prior to the IB-Stim treatment, Tayler’s parents hadn’t heard her laugh for months.
Now she cracks up regularly.
“Everything’s changed,” Tayler says. “I’m in a much better mood and the pain is so manageable. I get about one headache a week now in the spot where I was hit, but it’s nothing compared to what it used to be.”

Tayler thanks Drs. Chogle and Taraman for that.
“They’re both exceptional physicians and we’re lucky to have them,” she says.
Two-year clinical trial for IB-Stim and PCS
Dr. Chogle says the clinical trial, which will enroll patients between 12 and 18 years old, is expected to last two years.
“We’ll be evaluating symptoms and looking at objective biomarkers that are measurable,” he says. “If we can show a significant effect, which I’m hoping we will, this could have applications for kids who suffer concussions as well as adults — like NFL players. This could prove to be a very effective treatment option for them.”
To read more about the study, visit ClinicalTrials.gov and search for NCT number NCT04978571