Gene therapy at CHOC for rare metabolic disorders
Researchers at the Children’s Hospital of Orange County (CHOC) Metabolic Lab are leading the way in developing advanced treatment options, including gene therapy, for lysosomal storage disorders (LSDs). Unlike labs that are often removed from patients’ everyday lives, CHOC researchers’ lab work is intertwined with the multidisciplinary care provided in the Foundation of Caring Lysosomal Storage Disorder Program at CHOC, providing real-time context and motivation for their work.
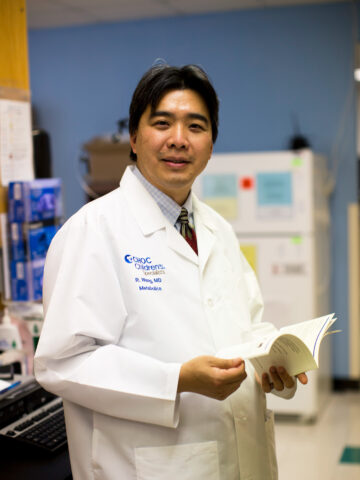
“Whatever we do, whether it’s a human clinical trial or the work we do in the laboratory, it is patient-focused,” says Dr. Raymond Wang, board-certified clinical geneticist, biochemical genetics specialist, director of the Lysosomal Storage Disorder Program and clinic director at the California Institute for Regenerative Medicine Alpha Stem Cell Clinic. “Every single research project we have in the laboratory essentially came from a question that one or more of our patients’ families asked in the clinic.”
Advanced lysosomal storage disorders treatment
LSDs are a group of approximately 50 rare inherited diseases characterized by lysosomal enzyme deficiencies, leading to abnormal substrate accumulation in the body. LSDs are progressive multisystem disorders with a variety of presentations. Currently, treatments are available for some LSDs, but none have cures.
Dr. Wang and his team at the CHOC Lysosomal Storage Disease Laboratory (Lyso Lab), part of the CHOC Metabolic Lab, are actively researching LSDs and leading multiple clinical trials for novel LSD treatments, many including gene therapy. Current work includes the following.
Mucopolysaccharidosis type I (MPS I)
MPS I leads to glycosaminoglycan build-up, causing a range of symptoms, including bone, eye and heart issues. The current available treatments for MPS I are stem cell transplant (for severe MPS I) and enzyme replacement therapy (for non-neurologic symptoms of MPS I).
The CHOC team is participating in a gene therapy clinical trial involving encapsulating the MPS I gene in a vector, similar to a viral shell, that, when placed in the central nervous system, equips other cells with the ability to make the missing enzyme. Five patients have now received this treatment at CHOC, more than at any other facility worldwide.
Pompe disease
Pompe disease causes glycogen buildup in the heart and skeletal muscles, typically leading to heart failure by 4 to 8 weeks of age. Enzyme replacement therapy is an approved treatment, effectively reversing heart failure and extending patients’ lives. However, new issues have been identified, including muscular diseases.
Investigators in the Metabolic Lab are conducting gene therapy research involving base editing to discover ways to address the muscular diseases they observed in patients receiving treatment in the Lysosomal Storage Disorder Program. The gene is now frequently able to be corrected in the lab.
Salla disease
Salla disease involves an accumulation of sialic acid, leading to neurological symptoms. Using base editing in cell models, the Lyso Lab has recently proven the ability to use base editing to correct 60% to 70% of abnormal genes.
The Lyso Lab is excited by these successes but continues to keep their eyes on the next steps and the overarching goal of making a meaningful difference in the lives of patients with LSDs.
“It’s awesome to say, ‘We corrected this in a high proportion of cells,’ but it doesn’t really help the patients yet,” Dr. Wang says. “The next goal is to take what we found in the cells to see if we can demonstrate the same kind of correction in an animal model of the Salla disease. We need to show that even as we’re making corrections, we’re not causing errors elsewhere in the genome. From there we can proceed on to clinical trials.”
Ultimately, Dr. Wang aims to find a one-size-fits-all approach to treat multiple conditions using the same gene therapy.
Discovering and answering new questions in newborn screenings
Due to the tremendous benefits of early diagnosis and treatment, the recommended panel for newborn screenings now includes MPS I and Pompe disease. These screenings have led to one MPS I diagnosis and several infantile-onset Pompe disease diagnoses, allowing identified infants to access treatment earlier than previously possible.
“Starting treatment in those kids has made a tremendous difference,” Dr. Wang says. “It’s just a few months, but those few months count tremendously. The babies we’ve treated almost from birth are in so much better shape than the ones who got sick and were in the ICU with heart failure before they received a diagnosis.”

However, early detection of rare conditions, such as MPS I and Pompe disease, opens the door to new questions for Dr. Wang and the CHOC team.
“The flip side to that is we found patients with much less severe disease as a result of the infant screenings,” Dr. Wang says. “It’s a learning process: How do we treat them if they’re not going to be quite so severe? But that’s part of the process. We’ll have to learn how to take care of those babies, as well.”
Research with a holistic perspective
The comprehensive, multidisciplinary Lysosomal Storage Disorder Program, combined with the Lyso Lab, provides an uncommon, multifaceted perspective for the CHOC research team.
“It’s rare to have so many people in one place who are not only good scientists, who not only have experience with genome editing, but who also have knowledge and experience in the course of diseases,” Dr. Wang says. “That’s what’s singular about our work. Everybody comes in with not just the technical expertise, but also the commitment to the patients.”
A common question when studying rare diseases
The CHOC team is often asked why they focus on rare conditions such as LSDs when there are common conditions without effective treatment options or cures. For Dr. Wang, the answer is clear.
“In studying the rare, you have the opportunity to take care of the common,” Dr. Wang says. “What we learn from these projects in rare diseases, including the methods and maybe even treatment processes, can then be applied to common diseases. You open a little bit of a vanguard and pilot something, make that work well and then apply it to something that can benefit greater society.”
Learn more about the Metabolic Lab at CHOC.
Learn more about CHOC’s Foundation of Caring Lysosomal Storage Disorder Program




