Among clinical conditions, sepsis – an infection of the bloodstream – is among the most grave and quick to take its terrible and gruesome toll.
The body becomes overwhelmed by a toxic cascade of inflammation.
Untreated, sepsis leads to leaky blood vessels, massive swelling, fluid in the lungs and, ultimately, organ failure and death.
Survivors sometimes need a liver transplant or are on dialysis for life and become intellectually disabled.
In January 2022, CHOC landed one of the nation’s top leaders in pediatric quality improvement and sepsis care, Dr. Raina Paul.
A physician researcher who specializes in emergency medicine, Dr. Paul, who came to CHOC from the pediatric emergency department at Northwestern Medicine and most recently Advocate Aurora Hospital in Illinois, was a chief architect of the Children’s Hospital Association’s Improving Pediatric Sepsis Outcomes (IPSO) collaborative.

Launched in 2016, IPSO includes 64 pediatric hospitals working together to decrease sepsis-associated morbidity and mortality using robust quality improvement science.
Difficult to diagnose
Around 45 in 100,000 children develop sepsis, a condition that is notoriously difficult to diagnose because there isn’t one particular lab test that tells you that you have it.
“You have to put multiple different pieces of data together,” Dr. Paul explains.
Time is of the essence in identifying and treating sepsis, which severely affects more than 75,000 children each year in the United States.
The mortality rate for kids 0 to 18 with sepsis is between 10 to 20 percent, and the rate of morbidity – disease, injury, and disability – is far higher, Dr. Paul says.
Getting those rates down is critical, and Dr. Paul’s research has identified gaps in care and ways to fix them.
“Quality improvement really appeals to me because it’s focused on how we can fix things now and how we can optimize evidence-based medicine and delivery, often in high-pressure settings,” she says.
A longtime interest in quality improvement science
Dr. Paul became interested in researching ways to use quality-improvement science to better pediatric sepsis care during her residency and fellowship at Boston Children’s Hospital from 2005-2011. She was among the first pediatricians to publish a paper on the topic during her training there as a resident and fellow.
“The timeliness of your intervention literally will save a life – that’s what our work demonstrated,” she says.
A graduate of the combined program in humanities and medicine at Albany Medical College in New York, Dr. Paul is one of four co-chairs who has been at IPSO – the largest pediatric sepsis collaborative in the world – from the start.
“Our goal is to really improve the timely therapeutics for sepsis that we know are important to saving lives,” she says.
As data chair for IPSO, Dr. Paul was responsible for developing all the metrics for the 64 hospitals in the collaborative. Clinicians study the electronic healthcare records (EHR) of patients and mine their vitals to determine if someone is at high risk of developing sepsis.
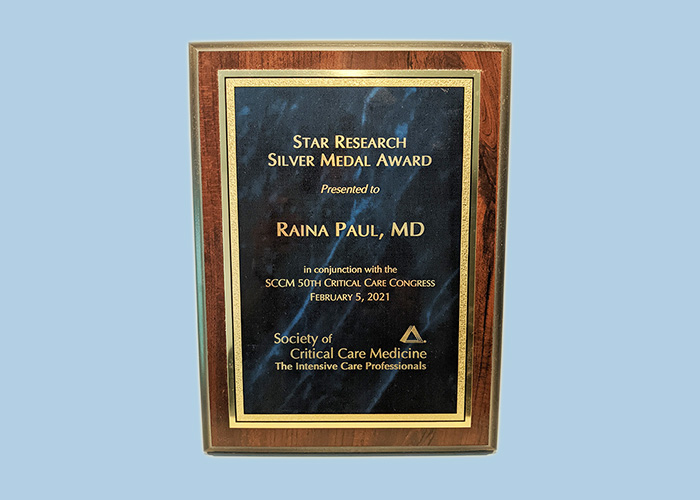
Award-winning research in emergency medicine
Dr. Paul’s latest sepsis study includes 256,000 patients through 2021 and is currently pending publication. Related publications have been published numerous times in Pediatrics and Annals of Emergency Medicine and have been presented on the national and international stage, winning multiple awards.
Since its formation in 2016, the IPSO collaborative has reduced the mortality rate for patients with sepsis to 3 percent from 6 percent, Dr. Paul says.
At Boston Children’s, Dr. Paul had installed in ED rooms large clocks that count down from an hour after a patient is diagnosed with sepsis. A similar “septic shock” clock was added to Cerner, one of the leading EHR platforms.
“Some people complain it’s gimmicky but it speaks to the unique situation in which we have to quickly deliver care for these patients,” says Dr. Paul, noting that several members of IPSO have adopted the same idea.
ISPO risk buckets and Child Hospitalization Early Warning Score (CHEWS)
Members of IPSO check the vitals of ED patients every four hours and clinically put a patient in risk buckets and then send automatic pagers or texts to the clinicians attached to the patient to alert them they need to go bedside.
“We’ve also included families and parents in that process,” says Dr. Paul. “We’ve piggybacked on the already existing infrastructure of the CHEWS (Child Hospitalization Early Warning Score) and either added, replaced, or modified it to include components for sepsis.”
A patient can arrive at an ED already experiencing sepsis or can acquire hospital-onset sepsis – something IPSO is working to reduce, if not eliminate.
“Anyone can get sepsis, especially if their immune system is weakened because of some other issue,” Dr. Paul says.
Dr. Raina Paul’s family and friends
Dr. Paul, who grew up in Toronto, has family in the Bay Area – part of the reason she decided to relocate to California and join CHOC.
Her husband, Dr. George Verghese, is a pediatric cardiologist who trained at Boston with her and is vice president of quality for Teladoc, the largest telehealth company in the country.
Dr. Verghese, who works part-time at Children’s Hospital Los Angeles, is regarded as a physician leader in health care quality measurement and improvement.
Dr. Paul has some good friends at CHOC. She has been close for over a decade with CHOC’s senior vice president and chief medical officer, Dr. Sandip Godambe, and she became fast friends with critical care specialist Dr. Juliette Huntduring their residency together.
But it was CHOC’s growing stature in pediatric healthcare that also brought Dr. Paul to Orange County.
“Over the past five years,” Dr. Paul says, “CHOC has been much more active in research in the quality scene and the optimization of metrics. I’ve been seeing CHOC everywhere. I think they’ve done an incredible job collating and recruiting the right people and creating the right infrastructure.”
CHOC also has a large population of patients to study in the hopes of creating the most optimal outcomes for children not just with sepsis, but a host of other diseases.
“We have the ability to affect so many patients and also to study so many of them,” says Dr. Paul, noting that CHOC’s ED will see well over 100,000 patients this year. Dr. Paul herself saw CHOC’s 100,000th patient in June.
An ‘exciting time’ to join CHOC
CHOC leaders are thrilled Dr. Paul has joined the team.
“Dr. Paul is already lending her strengths to CHOC to improve pediatric sepsis early identification in the Emergency Department and inpatient setting,” says Dr. Theodore Heyming, medical director of emergency medicine at CHOC.
“Her expertise in quality improvement has led to improved variable selection and outcome measures for CHOC’s current pediatric sepsis identification campaign and will improve overall sepsis care at CHOC,” he added.
Dr. Paul also has lent support to CHOC’s data science team to further improve CHOC’s current machine learning algorithm for sepsis identification in the ED, Dr. Heyming said.
“This is an exciting time for quality improvement at our facility, and I’m proud to have Dr. Paul as a member of CHOC,” he said. “Her efforts and support will make us a leader in pediatric quality improvement and sepsis care.”

CHOC Hospital was named one of the nation’s best children’s hospitals in seven specialties by U.S. News & World Report in its 2025-26 Best Children’s Hospitals rankings.